Esophageal Motility, Esophagus Reflux and Achalasia
There are three parts to swallowing which allows food from the mouth to enter the stomach and thus commence with the processes of digestion and absorption. The esophageal stage of swallowing is the last part and follows the pharyngeal stage which is preceded by the voluntary stage. The esophageal stage of swallowing, like the pharyngeal stage, is involuntary and coordinated by the autonomic nervous system.
Esophageal Peristalsis
The esophagus itself is a narrow muscular tube extending from the throat (pharynx) to the stomach. Its main function is to conduct food from the mouth to the stomach.This is done by two types of peristaltic contractions :
- Primary peristalsis
- Secondary peristalsis
Primary peristalsis is a continuation of the peristaltic wave that originates in the pharynx. It extends all the way to the stomach and is sufficiently effective to push the food from the pharynx to the stomach in less than 10 seconds. This occurs faster when assisted by the action of gravity if a person is standing or sitting upright.
Secondary peristalsis is the backup motility mechanism of the esophagus. It is triggered by distention of the esophagus due to presence of food (bolus ~ ball of food). Any food that has not passed into the stomach by the primary peristalsia will be pushed by repeated secondary peristaltic waves.
The passage of food through the esophagus is fairly rapid since food does not have to delay its transit in the esophagus for mechanical or chemical digestion. To aid with this speedy movement, the inner lining of the esophagus has simple mucus glands. The mucus secreted from these glands lubricate the surface between the bolus and the inner esophageal lining (mucosa).
Control of Esophageal Motility
Since primary peristalsis is a continuation of the peristaltic wave from the pharynx, it is essentially controlled by the areas that initiate and propagate the wave at this point. Impulses triggered by the presence of food in the mouth (tactile) sends feedback to the medulla oblongata through the trigeminal and glossopharyngeal nerves. The swallowing center located in the lower pons and medulla then sends motor impulses to the pharynx and upper esophagus through cranial nerves V (5 – trigeminal), IX (9 – glossopharyngeal), X (10 – vagus) and XII (12 – hypoglossal).
The secondary peristaltic waves are triggered by intrinsic reflexes of the enteric nervous system. It is backed up by motor impulses from the medulla which travels to the esophagus via the glossopharyngeal and vagus nerves. The ability of the myenteric plexus to initiate and maintain movement via the secondary peristaltic wave means that esophageal swallowing can continue independently without input from the central nervous system.
Movement of Food through the Lower Esophageal Sphincter (LES)
Similar to the peristaltic reflex in intestinal motility, the part of the esophagus distal to the bolus (ahead of the bolus in the direction of movement) relaxes, while the proximal part constricts. This is known as receptive relaxation and is propagated by the inhibitory neurons of the myenteric plexus. As food moves through the esophagus, this reflex extends well beyond the area immediately ahead of the bolus and may cause reflex relaxation all the way to the stomach and duodenum in preparation for the entry of food.
The lower end of the esophagus where contents empty into the stomach has a circular muscle sphincter known as the lower esopahgeal sphincter (LES aka gastroesophageal sphincter, cardiac sphincter). This sphincter is constantly constricted to prevent the gastric contents from entering and damaging the esophagus due to the action of gastric secretions, particularly hydrochloric acid. The sphincter’s protective function is backed up by the extension of the distal portion of the esophagus into the stomach. This acts somewhat like a valve. The receptive relaxation wave also relaxes the LES and allows the rapidly moving food to enter the stomach quickly.
What is Esophageal Reflux?
The esophagus is the muscular tube leading from the throat to the stomach. It directs and food and drink into the stomach for digestion and absorption which continues through the small intestine. Esophageal motility ensures that peristaltic waves that start in the throat during swallowing continues to propel the bolus (ball of food formed after chewing and pharyngeal swallowing) into the stomach.
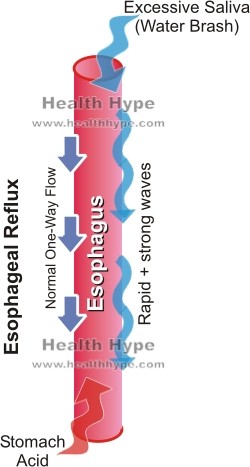
The direction of movement is from the throat to the stomach and retrograde flow (backward flow) is prevented by the direction of the peristaltic waves. In addition, the lower esophageal sphincter (LES) at the bottom of the esophagus ensures that the stomach contents do not travel up into the esophagus.
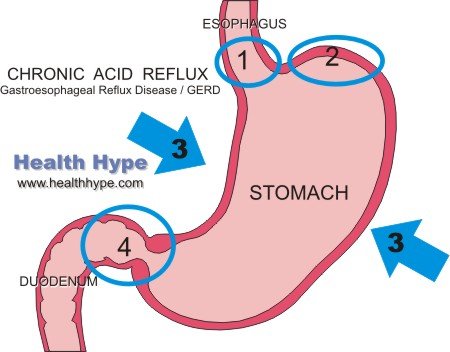
Esophageal reflux may be related to regurgitation or vomiting. Regurgitation is a more passive process than vomiting and can propel food in the esophagus, stomach or even first part of the small intestine back into the throat or mouth. Gastroesophageal reflux disease (GERD) is chronic acid reflux usually associated with lower esophageal sphincter dysfunction (LES). This is one of the more common causes of esophageal reflux. Other causes may be due to problems in the esophagus like a tumor, constriction, failure of the LES to function properly or dysmotility.
Symptoms of Esophageal Reflux
- Water brash – a sudden secretion of large amounts of saliva to neutralize the acidic stomach contents in the esophagus
- Nausea, sometimes leading to vomiting
- Heartburn – burning chest pain
- Indigestion – stomach bloating, excessive belching
- Throat irritation
- Projectile vomiting due to obstruction in the lower part of the esophagus, stomach or duodenum
Chronic reflux may lead to a host of symptoms in the upper airway, including coughing, hoarse voice and a lump in the throat feeling.
Causes of Esophageal Reflux
- Gastroesophageal Reflux Disease (GERD)
- Stomach contents, and sometimes duodenal contents, pass up into the esophagus.
- Occurs due to a failure of the lower esophageal sphincter to prevent the backward flow of stomach contents, hiatal hernia or increased intra-abdominal pressure.
- Achalasia
- Food cannot enter the stomach at a rate that allows for complete clearing of the esophagus.
- Occurs due to a failure of the lower esophageal sphincter to open fully.
- Esophageal Stricture
- An esophageal stricture is an abnormal narrowing of the esophagus.
- Occurs for various reasons including an obstruction like a tumor, inflammation of the esophageal wall, compression from an external structure or constriction due to scarring of the esophageal wall.
- Stomach or Small Intestine Obstruction
- An obstruction in the distal end of the esophagus (pylorus) or proximal parts of the small intestine may cause regurgitation and reflux.
- This may arise due to pyloric stenosis, tumors, foreign bodies, gallstones or other causes as outlined under blocked bowel.
What is Achalasia?
Achalasia is a rare condition where the movement of food through the esophagus and into the stomach is impaired due to failure of some of the esophageal muscles to relax. The lower esophageal sphincter (LES) which is a ring of muscles that control the passage of food between the esophagus and stomach are hypertonic meaning that it it remains contracted. Achalasia is an esophageal motility disorder in that the coordinated movement of foods through the esophagus (gullet) is impaired.
Causes of Achalasia
When food enters the esophagus, a series of coordinated muscle contractions known as the peristaltic wave pushes food down the esophagus. At the end of the of the esophagus, the LES (also known as the cardiac sphincter) should open and allow food to enter the stomach. The LES is an important structure that prevents the stomach (gastric) contents from emptying into the esophagus and causing damage due to gastric acid.
With achalasia, the peristaltic wave is disrupted and the LES does not relax and open. With time, the body of the esophagus becomes progressively dilated and this appears as a balloon-like esophagus (gullet) with a stricture at the bottom (LES) which can be seen upon conducting a barium swallow x-ray (refer to the picture below).

The cause of achalasia is unknown but certain findings have provided some answers as to how it occurs. There seems to be a defective release of nitric oxide by nerve cells that should prompt the LES to relax (inhibitory neurons). There also appears to be a degeneration of the myenteric plexus which innervates the esophagus. This indicates the the nerves signals to the muscles of the esophagus are impaired and cannot coordinate the opening and closing of the LES.
Symptoms of Achalasia
The most common symptom reported by achalasia patients is dysphagia (difficulty swallowing). This develops gradually and may only be noticed when consuming solid foods. In the early stages of achalasia, dysphagia may not be constant but rather occurs in episodes that passes on its own. Some patients initially report the symptoms as indigestion which eases after walking or standing up.
Regurgitation of food is a common feature as well as gagging. As the condition progresses, there is pulmonary aspiration where the esophageal contents enter the airways. This more frequently occurs at night (nocturnal) and may cause the patient to wake up coughing with a choking sensation. Aspiration can eventually lead to a host of respiratory symptoms and conditions.
There is a sensation of pressure in the chest just behind the breastbone (retrosternal) which may sometimes be described as heartburn although it is not due to acid reflux. Esophageal spasms result in chest pain. As the condition progresses, the patient may only eat semi-solid foods or drink liquids for nourishment. Loss of weight is eventually seen in most achalasia patients.
References
- Esophageal Motility Disorders. Medscape

