Eyelid Inflammation (Blepharitis)
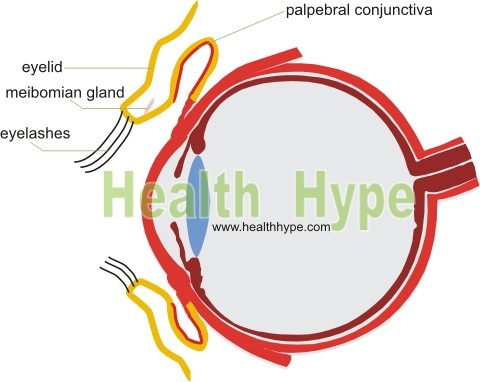
The eyelids are protective flaps that shield the eyes. It also helps to spread out tears over the eye. The eyelids are delicate yet effective shielding structures and is made up of several layers. It is covered by skin with the inside lined by a continuation of the conjunctiva known as the palpebral conjunctiva. Underneath the skin is a subcutaneous layer that overlies the orbicularis oris muscle, palpebral ligament and a thickened connective tissue plate known as the tarsal plate. The upper eyelid (palpebra superior) is larger than the lower eyelid (palpebra inferior). A specialized sebaceous gland in the rim of the eyelid secretes an oily substance known as meibum. Hairs extending from the borders of the eyelids (eyelashes) serves to further protect the eye from dust and debris that can injure the eye tissue.
What is blepharitis?
Blepharitis is the term for inflammation of the eyelids. It is a common condition and most of the time blepharitis affects the edge of the eyelids. Inflammation may occur on the outer front part of the eyelid in which case it is known as anterior blepharitis. Alternatively it may be present on the inner back side of the eyelid which is in contact with the eyeball and is then referred to as posterior blepharitis. When the skin of the eyelid is affected, it is is known as blepharodermatitis. If the eyelid and conjunctiva lining the eyeball are both affected then it is referred to as blepharoconjunctivitis. The term dermatoblepharoconjunctivitis indicates that the inflammation is affecting the skin, inner eyelid tissue and conjunctiva.
Another condition known as blepharochaliasis (picture below) is characterized by recurrent episodes of eyelid inflammation. Over time this causes the eyelid tissue to become thin and wrinkled. It is a rare condition that arises due to unknown causes. It almost always affects only the upper eyelids.
Picture of blepharochaliasis from Dermatology Atlas (www.atlasdermatologico.com.br)
Courtesy of Samuel Freire da Silva, M.D.
Types of Blepharitis
Blepharitis can be categorized as acute or chronic. Acute blepharitis is mainly infectious or allergic in nature. It tends to affect the edge of the eyelid near the eyelashes and can be further classified as ulcerative or non-ulcerative. This means that there may be ulcer (open sore) formation associated with the inflammation or just inflammation on its own without ulcer formation. Acute ulcerative blepharitis is most commonly due to bacterial infections while acute non-ulcerative blepharitis is more often caused by allergies. Chronic blepharitis is due to unknown causes but usually not associated with an infection. There does, however, appear to be an associated risk with chemical irritants, including fumes and vapors. It is persistent and difficult to treat and may be associated with recurrent episodes of other eyelash disorders like a hordeolum and chalazion.
Classification of blepharitis based on the cause may also be associated with different clinical presentations.
- Acute infectious blepharitis is most commonly caused by bacteria, particularly staphylococci. It is therefore referred to as staphylococcal blepharitis. These bacteria occur naturally in the area but its population is usually carefully controlled. However, its population can grow rapidly and become pathogenic.
- Seborrheic blepharitis is associated with seborrheic dermatitis and this skin disorder is commonly seen on the scalp and eyebrows. It is commonly referred to as dandruff. Although the exact cause of seborrheic dermatitis is unknown, it is often associated with the yeast (fungus) Malassezia furfur.
- Meibomian blepharitis is a result of blockage of the meibomian glands (oil glands in the eyelids). As these glands are located more towards the back of the eyelid, it tends to cause posterior blepharitis. The ensuing inflammation can extend to the conjunctiva and even cornea (keratoconjunctivitis).
It is not uncommon for there to be a combination of the different types of blepharitis especially as secondary bacterial infections can affect an existing case of seborrheic or meibomian blepharitis.
Causes of Blepharitis
- Bacterial infection – particularly staphylococci
- Viral infection – herpes simplex or varicella zoster
- Seborrheic dermatitis (dandruff)
- Rosacea
- Molluscum contagiosum
- Meibomian gland dysfunction
- Allergies
- Parasites like Phthiriasis palpebrarum (‘crabs’ or pubic lice on the eyelids) or Demodex mites
Signs and Symptoms
Blepharitis presents as red and swollen eyelids which is sore and often itchy. Most of the time this is limited to the edges of the eyelids. In infections, the pustules on the edge of the eyelid coalesce and ulcerate (shallow open sore). The eyelashes may fall off (trichiasis) or be skewed from its normal alignment (misdirected). Usually both eyes are affected simultaneously although it can occur unilaterally (one side only). Excessive oiliness of the eyelid skin with flaking or scaling skin is typically associated with seborrheic dermatitis. A sticky discharge and crust formation often forming over the eyelids at night may also be present.
There may be redness of the eyes with excessive tearing and a burning sensation depending on the type and severity of the condition. The tears may be of a different consistency particularly when the meibomian glands are affected. Sometimes there is dryness of the eyes. Sensitivity to light (photophobia) is often present as well. Symptoms of eye strain, with a grittiness or foreign body sensation and blurred vision may also accompany the eyelid inflammation. If left untreated, corneal ulceration may occur.
Treatment of Blepharitis
The underlying cause of the blepharitis should be ascertained and the treatment prescribed accordingly. Bacterial infections require antibiotics – topical and/or systemic. Corticosteroids may help reduce the inflammation. The focus should be on eye hygiene – proper cleaning involving a warm compress, gentle massage of the eyelids and washing with water and a hypoallergenic soap or even diluted baby shampoo. Care should be taken not to exacerbate the condition by this cleansing process and one should follow the attending doctor’s advice. Underlying diseases such as seborrheic dermatitis and rosacea need to be treated accordingly.