Frostbite (Freezing Injury) Causes, Symptoms, Treatment
What is frostbite?
Frostbite is a injury caused to tissue by extreme cold. This type of cold injury causes the tissue to freeze which means that fluid within the tissue crystallizes. Frostbite is preceded by a milder reversible tissue injury known as frostnip. As this worsens, frostbite sets in. Depending on the severity, frostbite can lead to permanent tissue injury and sometimes even the loss of affected parts of the body.
Freezing injuries occur with exposure to very cold conditions, especially where there is snow and wind. The extent of the injury also depends on the duration of exposure to the cold. Frostbite has become less common in cold climates where residents are aware of the potential dangers. However, it still occurs in people who are not acclimatized to the cold weather and do not wear the proper thermal protective clothing.
Causes of Frostbite
Frostbite occurs as a result of cold exposure or when the affected tissue drops to very low temperatures for other reasons. Therefore frostbite may be a result of:
- Cold and windy weather.
- Immersion in water for long periods.
- Clothing that is wet or too tight.
- Direct contact with ice or very cold fluids.
- Touching freezing metals.
The body has several mechanisms to regulate the internal temperature. Although the skin has insulating properties, it is not impervious to extremes of temperature. Circulating blood usually prevents surface parts of the body from becoming too cold.
However, low temperatures also causes the blood vessels on the surface to constrict (narrow). This reduces blood flow and therefore warmth to the surface. As a result the body is not able to prevent freezing injuries to the surface beyond a certain point.
How cold for frostbite to occur?
Freezing injuries like frostbite can occur in varying low environmental temperatures. Normally the blood flow to the skin varies between 200 to 250 mL/min. At 15ºC (approximately 60ºF) the blood flow drops to 20 to 50 mL/min. Once the temperature drops below 15ºC, the blood flow to the skin occurs in short bursts every few minutes that lasts for short periods of time, like 5 to 10 minutes.
As the temperature drops below 10ºC (50ºF) nerve injury occurs and there is loss of sensation on the skin. Once the surface temperature falls below OºC (32ºF), blood flow to the skin surface is almost zero and the tissue freezes. There the onset of frostbite depends on how long the surface temperature can be maintained at a level that allows for sufficient blood flow to prevent freezing injuries.
Signs and Symptoms
Freezing injuries like frostbite occurs in stages. The initial stage is frostnip. This is followed by superficial frostbite if the cold exposure continues and eventually to deep frostbite which is the most severe form. Frostbite is also classified into four degrees, with the first being frostnip, the second being superficial frostbite, and the third and fourth being deep frostbite.
Superficial Frostbite
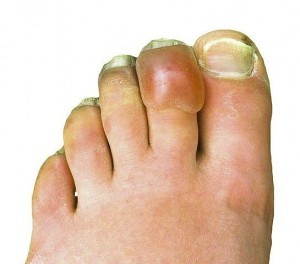
Frostnip is the mildest of the injuries and affects only the outermost layers of the skin. The area feels cold and initially becomes red and then progresses to paleness. Eventually the area turns white. There is a prickling feeling at first, then pain and eventually numbness. The tissue starts to harden and has a waxy appearance.
Deep Frostbite (Severe)
At this stage the deeper tissue including the area lying underneath the skin is affected. This can extend to the muscles, joints and blood vessels.The pain may intensify but usually there is numbness as the condition worsens. The tissue dies and gangrene may develop if the cold exposure persists.
Frostbite Blisters
If the progression of frostbite is interrupted by rewarming, even if it is not done medically, then certain symptoms may start. Blisters are one of the common signs of rewarming during frostbite. Smaller fluid-filled blisters follow after rewarming from superficial frostbite. Larger blisters, which are sometimes blood-filled, tend to form after rewarming from deep frostbite.
Treatment of Frostbite
The treatment of frostbite is not always simply a matter of rewarming the area. Although this is an important measure, it is also important to remove the cold exposure and prevent heat loss. With rewarming the blood vessels widen and blood flow should return to the area. However, this may need to be expedited at times. Similarly the oxygen levels in the affected tissue may need to be increased beyond that which is carried through the blood.
Prevent Freezing
It is important to first prevent further freezing. The source of the cold should be removed, like removing the affected portion from water or removing wet clothing. It is also important too immediately treat hypothermia, which is often present. Once further freezing can be prevented, then only should rewarming be commenced. Pain medication may be administered as there is often intense pain that arises when the tissue is rewarmed.
Rewarm Area
Removal of the cold source can lead to rewarming on its own or further measures may need to be taken. The affected area should be placed in warm water, around 37º to 42º C (99º to 108º F). Never use hot water or a direct heat such as warming the area by a fire or stove. These heat sources can cause further tissue damage. Immersion in warm water should only be for 15 to 30 minutes.
Remove Tissue
Rewarming does not mean that all of the affected tissue can be saved. Dead tissue has to be removed to aid with healing of the living but injured tissue. Similarly infected tissue needs to be removed as well. This process of tissue removal is known as debridement and should be done by a medical professional.
Other Measures
- Whirlpool therapy helps with blood circulation and removal of dead surface tissue.
- Hyperbaric oxygen therapy helps with increasing blood oxygen levels.
- Wound therapy helps with the prevention of infection and aids healing of injured tissue.
- Amputation is reserved for severe cases to remove the affected area where the tissue may be decaying.
Medication
- Painkillers to manage the pain that arises during rewarming.
- Antibiotics to treat bacterial infections that arise as a complication.
- Clot-busters to breakdown clots and assist with restoring blood flow.
References: