Gastroparesis (Stomach Paralysis and Slow Stomach Emptying)
Normal Stomach Activity
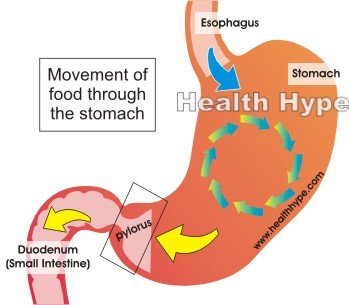
The stomach is a hollow sac with muscular walls that can contract and relax in order to help with digestion and motility. Food enters the stomach after passing down the esophagus (food pipe). Once in the stomach, the food needs to be crushed (mechanical digestion) and churned with digestive enzymes (chemical digestion). Eventually the partially digested food mixed with digestive enzymes, gastric acid and water is passed out of the stomach and into the first part of the small intestine known as the duodenum. This semi-fluid mass is known as chyme.
The movement of the chyme into the duodenum is carefully controlled by the action of the stomach muscles through the narrow terminal part of the stomach known as the pylorus. It is regulated by the opening and closing of the pylorus in a manner that is referred to as the pyloric pump while the muscles in the other parts of the stomach pushes the chyme through it. This process is known as gastric emptying. In this way only chyme passes into the stomach and undigested food remains in the stomach for further crushing and churning. The entire process is regulated by the certain nerves and hormones that control the action of the stomach muscles, pyloric valve of the stomach as well as the enzymes, acid and water in the stomach.
What is gastroparesis?
Gastroparesis is a condition where there is a delay in the stomach passing out its contents into the small intestine. Therefore the condition is also known as delayed gastric emptying. The main problem in gastroparesis is that the vagus nerve which controls normal stomach emptying is damaged or not working properly. It is a common condition seen in disease like diabetes mellitus where the vagus nerve is damaged over time. There are various other causes which are not as common – some may affect the nerve activity without damage to the nerve or the muscles of the stomach wall. Since the crushing of food and churning along with emptying are all hampered, food stays in the stomach for long. This leads to a range of stomach symptoms.
Meaning of Gastroparesis
Gastroparesis literally means stomach (gastro-) paralysis (paresis). It is a partial rather than complete paralysis. The vagus nerve which is a cranial nerve (CN X), meaning that it emanates directly from the brain, supplies the muscles in the stomach. With parasympathetic stimulation by impulses via the vagus nerve, the movement within the stomach (peristalsis) increases and the pyloric sphincter opens. This pushes out the chyme into the duodenum.
Understandably any disruption with the vagus nerve where there is decreased stimulation to the stomach will slow down this process. The stomach movements are drastically hampered and chyme does not pass out into the duodenum at a normal rate. The term paralysis can be mislead because the gastric emptying is delayed but does not cease entirely. Essentially this means that the mechanical activity of the stomach and particularly the emptying is slower than normal. Hence the term slow stomach is sometimes used to describe delayed gastric emptying and gastroparesis. It is important to note that the delay in gastric emptying is not due to any physical obstruction like a tumor which is more correctly referred to as gastric outlet obstruction.
Gastroparesis Causes
The most common cause of gastroparesis is diabetes mellitus (sugar diabetes). It may also be commonly seen with the use of certain medication, narcotics and after surgery. However, a large number of cases occur for no known reason. There are also several other causative factors including diseases that do not specifically affect the stomach muscles or nerves.
Diabetes
Gastroparesis is most commonly seen in diabetics. High blood glucose levels seen with diabetes mellitus, particularly if it is over a long period and poorly controlled, can damage all types of cells in the body. The tissue of the nerves are damaged and so are the blood vessels supplying oxygen and nutrients to the nerve tissue, further compounding the damage to the nerves. This type of damage to the nerves is known as diabetic neuropathy.
The lower part of the gut also has dysfunctional motility in diabetes mellitus thereby complicating the delay in gastric emptying even further. It is important to note that the symptoms of gastroparesis are common to many different disorders of the gut. The presence of these symptoms in diabetes mellitus should not be assumed to be due to gastroparesis until the appropriate investigations can confirm the diagnosis. Gastroparesis, or more correctly gastroparesis diabeticorum, is a problem in diabetes that develops after long periods of time.
Drugs and Surgery
Certain medication and substances can disrupt the nerve activity that controls the muscles in the stomach wall. Pain medications, certain types of antidepressants and calcium-channel blockers for high blood pressure and migraines are among the most common medication to cause this delay in gastric emptying. Some of this medication is used in respiratory, gastrointestinal, urinary and sleep disorders known as anticholinergic drugs may also be responsible as well as certain narcotics. Most of these drugs essentially slow down or decrease the activity of nerves mainly by interrupting the flow of chemicals between nerves or nerve endings and muscles.
Chemotherapy used for the treatment of cancer may also lead to gastroparesis and this is known as chemotherapy-induced gastroparesis. It may also occur with radiation therapy in cancer particularly if it is targeting tumors in the chest and abdomen. Sometimes the vagus nerve is unintentionally damaged during surgery particularly with procedures involving the stomach and surrounding structures.
Other causes
Gastroparesis may also occur in eating disorders like anorexia nervosa and bulimia. It is usually seen after long periods of time and is one of the main complications of these eating disorders.
Disorders that affect the functioning of the nerves and smooth muscles can also lead to gastroparesis. This includes conditions such as Parkinson’s disease, scleroderma, strokes, brain injury and abdominal migraines.
Other causes may not be due to any disease of the stomach muscles or nerves but slow down its normal processes. This may occur in pancreatitis, with imbalances in the levels of electrolytes (calcium, potassium and magnesium) or thyroid disease (hypothyroidism).
Gastroparesis may be seen after certain viral infections. It can be acute or sometimes chronic. These infections do not always specifically target the vagus nerve or stomach and the exact mechanism by which gastroparesis occurs in this instance is not clearly understood.
A significant number of cases occur for no known reason despite comprehensive medical investigations. These cases are known as idiopathic gastroparesis.
Gastroparesis Symptoms
The symptoms of gastroparesis are not specific for this condition. It is seen with many common stomach disorders. The slow emptying of the stomach contents means it stay in the stomach for longer where it can irritate the stomach lining, stretch the stomach wall, be regurgitated and even ferment with increased microbe growth in the stomach.
These symptoms include :
- Sensation of fullness (bloating) even after small meals
- Nausea
- Vomiting
- Abdominal distention (enlargement)
- Heartburn
- Abdominal discomfort or pain mainly in the middle and left side of the upper abdomen
- Lack of appetite
- Weight loss
- Nutritional deficiencies
- Fluctuations in blood glucose levels
Gastroparesis Diagnosis
Gastroparesis is diagnosed by assessing the movement of food through the stomach. This may be done with investigations like a gastric emptying study where a small amount of radiocontrast dye is ingested with food. The movement of this food can then be monitored with a scanner that tracks the radioactive material. Other methods to track the movement through the gut and highlight the stomach on x-ray is a barium meal or barium x-ray.
Upper GI endoscopy allows for the inside of the gut to be seen by inserting a long flexible tube with a light source and camera at the end through the mouth. This may help identify any obstruction or diseases that may be contributing to gastroparesis. A more specialized test which is not available at all health care facilities is a an electogastrogram (EGG). This measures the electrical activity of the stomach muscles when it contracts and relaxes.
Gastroparesis Treatment
The key to managing gastroparesis is with diet and medication. The cause of the gastroparesis should be treated as far as possible although in some instances the damage to the stomach nerves and muscles may be permanent. In severe cases where diet and medication is not providing significant relief, gastroparesis surgery may be considered.
Diet
Dietary modification may not be necessary in very mild cases although a person with gastroparesis should avoid large meals. The main components of a gastroparesis diet includes :
- Eating many small meals throughout the day – between 4 to 6 meals.
- Avoid fatty foods which tends to slow down digestion even further.
- High fiber foods must also be avoided as it slows down digestion and bulks up with water in the gut.
- Water intake during the course of the meal aid with movement in the gut and stomach emptying.
- Opt for semi-fluid or fluid meals like soups and low-fat shakes if solid meals worsen symptoms.
- Gentle walking after a meal may aid with digestion.
Medication
The two main drugs used for gastroparesis are metoclopramide and erythromycin (an antibiotic). These drugs increase stomach emptying but due to the side effects its use has to be carefully monitored. Other medication are used for controlling the symptoms of gastroparesis like antiemetics to ease nausea and vomiting. Two other drugs that aid with stomach emptying are domperidone and cisapride. Domperidone is not approved for use in the United States and cisapride was removed off the market and is available again but its use is restricted. Both drugs are associated with serious side effects.
Surgery
Surgical procedures are reserved for severe cases of gastroparesis where the symptoms are not easing and there is a risk of other serious complications arising. These procedures may involve the placement of tubes for venting trapped air in the stomach and/or nutritional supplementation. Sometimes the lower portion of the stomach may be removed and the remaining part joined to the small intestine. In rare cases, the stomach may be bypassed or removed altogether.