Heart Damage With A Heart Attack (Permanent and Irreversible)
A heart attack, or myocardial infarction (MI), is the death of a portion of the heart wall when there is an interruption in its blood supply. The heart wall is composed of three layers – the inner lining (endocardium), middle muscle layer (myocardium) and outer lining (epicardium) – and has its own supply of oxygen and nutrient-rich blood via the coronary arteries. There is usually underlying disease of the coronary artery, like atherosclerosis, where fatty plaques build up in the arterial wall. This is known as coronary artery disease and reduces the blood flow to portions of the heart wall. It is often asymptomatic if the extent of occlusion is less than 75% of the diameter of the arterial lumen.
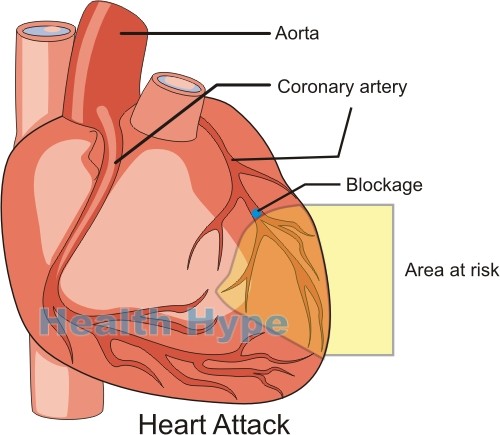
However, once there is a severe blockage or total occlusion then there is a wide range of symptoms that arise particularly when the heart muscle needs increased blood flow like during physical activity. This interruption in the blood supply causes muscle injury known as myocardial ischemia but the tissue does not die. It may persist for months or years without a heart attack and is known as ischemic heart disease. Eventually, the fatty plaque may become unstable and possibly rupture. This causes the formation of a blood clot at the site which completely occludes the artery and causes death of any tissue supplied beyond that point (myocardial infarction). A heart attack (myocardial infarction) is a serious clinical event that can cause death although not all heart attacks are fatal. Advancements in medicine and rapid response of emergency medical services has drastically reduced the mortality rate.
Extent of Tissue Death in a Heart Attack
Within the first 30 minutes, much of the damage is reversible if there is early intervention. After this time, the injury is usually irreversible with permanent damage to the tissue and subsequent necrosis (tissue death). Microscopic and macroscopic changes over minutes, hours, days and even weeks which severely compromises heart function as outlined under complications after a heart attack. The extent of the damage and its effects on cardiac functioning depends on a myriad of factors including :
- Size of the area supplied by the now occluded portion of the coronary artery.
- Location of the obstruction in the coronary artery.
- Severity of the obstruction – complete or partial (generally greater than 75% but typically above 90%).
- Rapidity of the obstruction – how quickly did the obstruction occur?
- Duration of obstruction – how long has the obstruction been present?
- Collateral supply of blood to the area at risk – alternate blood flow to the affected area.
- Needs of the affected portion – oxygen and nutrients.
- Spasm of the coronary artery (when present), the location and severity of the spasm.
- Cardiac demands – activity of the heart at the time.
- Heart rhythm and irregularity of the heart beat (arrhythmia).
- Blood oxygen levels.
Part of the Heart Affected in a Heart Attack
Layers of the Heart Wall
The part of the heart that is most affected in a heart attack is the myocardium. It is a thick muscular layer that constitutes most of the heart wall. The myocardium is also the most active and needs a constant supply of oxygen and nutrients to continue pumping blood efficient. If the myocardium fails to function, the beating heart ceases. In a heart attack, the entire myocardium is usually not affected simultaneously. Only the portion of the heart which has a severe interruption of blood supply is affected.
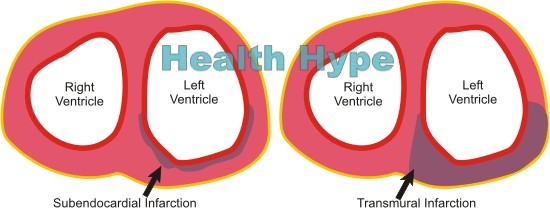
Thickness of the Heart Wall
The tissue just beneath the endocardium (inner lining of the heart) known as the subendocardium is the part that is initially affected. Gradually the damage to the myocardium extends outwards consuming greater portions of the muscular wall. An infarct may be isolated only to the inner one-third or half of the thickness of the heart wall and this is known as a subendocardial infarction. If it involves the entire heart wall, then it is known as a transmural infarction.
Most infarcts involving complete occlusion of a coronary artery causes transmural infarction. If the occlusion is partial but severe, then it may only result in a subendocardial infarction. An infarct that arises with shock may cause a subendocardial infarction of the entire wall. Intramural coronary artery disease (small vessels) may cause micro-infarcts throughout the heart wall.
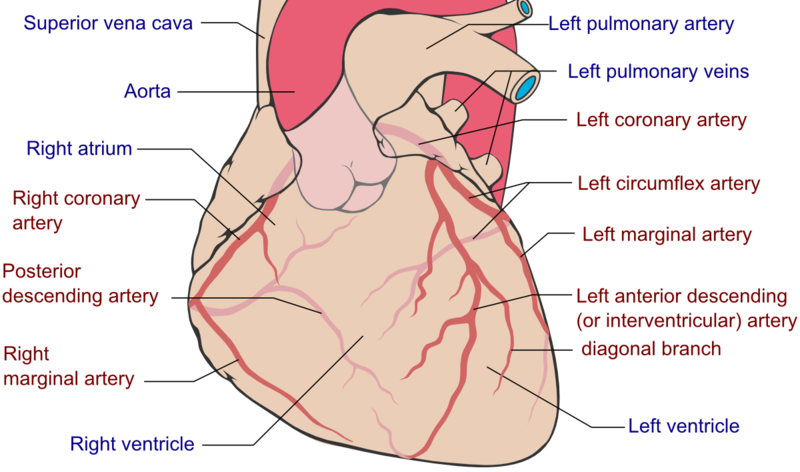
Area of the Heart Wall
It is important to understand the coronary circulation and coronary artery dominance as outlined under blood supply to the heart. Most infarcts affects the wall of the left ventricle and this is dependent on the artery that is compromised as indicated by the area of risk in the diagram above. Majority of heart attacks associated with occlusion of the coronary artery involves the anterior descending branch of the left coronary artery followed by the right coronary artery and the minority of cases involve the circumflex branch of the left coronary artery. An obstruction may occur more proximally or distally in the coronary circulation but is not as common.
Picture from Wikimedia Comons
- When the left anterior descending coronary artery is blocked, then the infarct may affect the anterior wall of the left ventricle, anterior aspect of ventricular septum and/or apex of heart.
- When the right coronary artery is blocked, then the infarct may involve posterior wall of the left ventricle, posterior aspect of the ventricular septum and may extend to the posterior wall of the right ventricle.
- When the left circumflex coronary artery is blocked, then the infarct may involve the lateral wall of the left ventricle.
Visible Changes in the Heart Wall
Microscopic changes are evident in the earliest stages of a heart attack. However, visible changes may only be evident after 4 hours. This initially presents as dark spotting or blotches in the area of the infarct right up to 24 hours after the infarct. Gradually the center of the infarct becomes yellow to tan in color while the border changes from a dark red to a red-gray margin which may occur over a period of 10 to 14 days. Finally scar tissue forms at the site after the second week until scarring is complete after month 2 following an infarct. This scarring will be present permanently. The size of the infarct is dependent on multiple factors as discussed above under extent of tissue death.