Placenta Problems – Infected Placenta and Low Placenta (Previa)
The Placenta
The placenta is the structure that connects the fetus to the uterine wall and is the conduit for nutrition and oxygen to reach the growing fetus. Essentially the placenta is the communication point between the mother’s blood circulation and that of the developing fetus.
Formation of the Human Placenta
The ovum (egg cell from a woman’s ovary) is fertilized by sperm (from the male after intercourse) in the fallopian tubes of a woman’s body. After fertilization, it takes the fertilized ovum several days (approximately 3 to 5 days) to reach the uterine cavity. During this period it grows to a ball of cells known as a blastocyte. While the fertilized ovum is unattached to the uterine wall, it is sustained by nutritious secretions from the fallopian tube and endometrial lining of the uterus. Once in the uterine cavity, the fertilized ovum is ready to implant on the wall of the uterus.
Trophoblastic cells on the surface of the ovum secretes proteolytic enzymes that digest the endometrial cells lining the uterine wall creating a suitable surface for implantation. Trophoblastic cords then extend from the surface of the fertilized ovum to attach to the endometrial lining. Blood vessels grow into these trophblastic cords that further develop as projections into the endometrial lining known as placenta villi or chorionic villi. Eventually these blood vessels in the placenta villi lie close to the blood sinuses around the mother’s blood vessels. The blood circulation of the mother and fetus now have a contact area to exchange nutrients, gases and waste products.
Blood from the endometrial arteries (spiral arteries) circulate around these placenta villi and exchange of nutrients and gases occur through the intervillous space. Blood carried by this villi is returned to the fetus through the umbilical vein. In this way, the fetal and maternal blood never actually mix.
Functions of the Human Placenta
The placenta has multiple functions all of which develop and sustain the fetus. These functions include :
- Nutrition. Nutrients in the mother’s blood stream can diffuse into the fetal circulation. These nutrients are derived from the food that the mother eats, digests and absorbs and nourishes the growing fetus.
- Gas exchange. Oxygen from the mother’s blood stream can diffuse into the fetal circulation where it is used for energy production. Carbon dioxide from the fetus diffuses into the mother’s circulation to be carried away and expelled by the lungs and kidneys.
- Immunity. Antibodies from the mother are delivered to the fetus through the placenta, and this protects the fetus and child for a period of time after birth until the child’s own immune system matures.
- Endocrine. The placenta produces and releases several hormones that aid the fetal growth and influence the mother’s body to sustain the fetus, prepare for childbirth and nourish the baby after birth. These hormones include human chorionic gonadotropin (hCG), human chorionic somatomammotropin and the female hormones estrogen and progesterone.
Infected Placenta
An infection of the placenta is known as chorioamnionitis. This term actually describes an infection of the chorion, amnion, amniotic fluid and/or placenta. It is also known as an intra-amniotic infection. An infected placenta can jeopardize the pregnancy and even the health of the mother.
An infection in the placenta can develop when bacteria enter through the birth canal (ascending infection) or by reaching the placenta through the mother’s blood stream (hematogenous). Most ascending infections are due bacteria although other pathogens may be involved, especially in hematogenous infections. The amniotic fluid may become cloudy and purulent with infiltration by leukocytes. This causes swelling of the tissue (villitis) and vascular congestion.
The infection can lead to preterm labor and premature rupture of membranes (PROM). Other complications in the fetus may include a lower apgar score (< 3) upon delivery, sepsis, respiratory tract infections like pneumonia, meningitis, cerebral palsy, seizures and even death. The complications for the mother may include bacteremia, pelvic abscess, post partum hemorrhage, pelvic abscess, poor wound healing and infection and thromboembolism.
Causes of an Infected Placenta
Most cases are due to an ascending bacterial infection and often the same bacteria involved in other urogenital infections are responsible for chorioamnionitis. The vagina and cervix maintain a microenvironment that prevents infections from reaching the uterus. This may be compromised thereby allowing pathogenic bacteria or even an overgrowth of healthy bacterial flora from reaching the placenta. Other risk factors may include poor urogenital hygiene, a short cervix and immunocompromised patients, like in HIV positive mothers.
While hematogenous spread of various pathogenic bacteria is possible, typically hematogenous infections that result in an infected placenta arise due to the TORCH infections :
- Toxoplasmosis
- Others like syphilis, tuberculosis, listeriosis
- Rubella
- Cytomegalovirus (CMV)
- Herpes simplex virus (HSV)
Symptoms of an Infected Placenta
The clinical presentation can vary with only a few symptoms of low intensity present in some mothers. Diagnosis may therefore be confirmed with follow up blood tests like a complete blood count (raised WBC count) apart from the presence of clinical features. Some of the signs and symptoms of a placental infection includes :
- Abnormal vaginal discharge – may be yellow to green in color with a foul odor
- Abdominal/pelvic tenderness (uterine)
- Fever
- Rapid heart rate (tachycardia) – mother (> 100 bpm) and/or fetus (>160 bpm)
At other times the symptoms are not typical of an infected placenta and the diagnosis can be missed without further investigation. Although an amniocentesis is avoided as far as possible, it may be necessary for a diagnosis in a subclinical infection.
Treatment of Placental Infection
Broad spectrum IV (intravenous) antibiotics are necessary to prevent maternal and fetal complications. This may be administered before assessing the results of a culture. The antibiotics may be continued by both mother and baby after birth, and the type of antibiotic used on both patients may differ. In acute chorioamnionitis, immediate delivery may be necessary especially if there are signs of fetal distress. However, this is dependent on the stage of pregnancy.
Placenta Previa
Placenta previa is the term when the placenta implants low in the uterus (womb), either partially or completely covering the cervix, or it may not cover the cervix at all. It is an uncommon but major complication of pregnancy. A placenta previa can lead to bleeding during or immediately after delivery.
How does a placenta previa occur?
Implantation of the placenta in the lower parts of the uterus is not uncommon in the early stages of pregnancy while the uterus is relatively small. This changes during the course of pregnancy as the growing uterus redefines the position of the placenta in the distended uterus. By the second to third trimester of pregnancy, the placenta is located in the mid to top of the uterus. With placenta previa, however, this does not occur and the placenta is low lying in the uterus and may involve the cervix as well.
The placenta is the conduit for nutrients and oxygen from the mother’s blood stream to reach the fetus. It only dislodges after delivery of the baby as the contracting uterus shrinks to a smaller size and shears away the placenta. If the placenta is blocking the cervix, the baby cannot travel down the birth canal during delivery.
The uterine muscles are arranged in a manner that allows it to constrict the the blood vessels of the uterine wall. This ensures that uterine contractions after delivery constricts the mother’s blood vessels that were communicating with the placenta. This mechanism ensures that there is only minimal post partum hemorrhage and is further backed up by the action of clotting factors in the blood. With a placenta previa, however, this mechanism is disrupted as the cervix and lower segment of the uterus thins (atrophy) prior to delivery and the uterine contractions cannot constrict the blood vessels.
Types of placenta previa
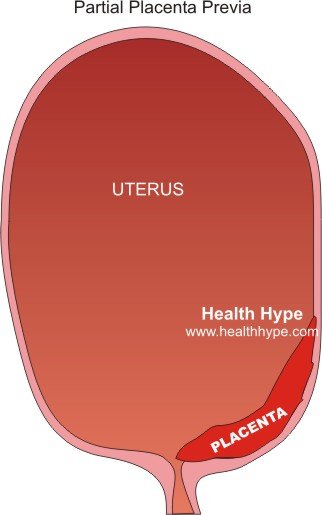
Placenta can be one of three types :
- Marginal where the placenta is on the cervix, near the border of the os (cervical opening) but is not covering it.
- Partial where the placenta is only partly covering the cervical opening.
- Complete where the placenta is totally blocking the cervical opening.
Symptoms of Placenta Previa
Vaginal bleeding and occasionally uterine contractions are the only two symptoms that will be seen with a placenta previa. It is may be diagnosed upon conducting a pre-natal ultrasound although the mother has not experienced any symptoms.
Bleeding
The characteristic feature of a placenta previa is painless, bright bleeding after the first trimester. It is more likely to be placenta previa if the bleeding occurs from the second half of the second trimester onwards. The vaginal bleeding may vary from light spotting to a heavy flow. It can be intermittent, stopping spontaneously and then recurring after a few days or weeks.
Contractions
Some women with placenta previa will experience uterine contractions with the vaginal bleeding. The contractions may cause abdominal discomfort or even a cramping pain but this is not as intense as labor pains. Uterine contractions may only be seen in 1 out of 5 women with placenta previa.
Low Placenta
A low lying placenta is known as placenta previa and means that the placenta is located lower down the uterus near or over the cervix. Normally the placenta is positioned higher up the uterus by the second to third trimester. This ensures that the birth canal is unobstructed for delivery.
The placenta is a communication point for the circulation of the mother and fetus. Nutrients and oxygen are transported to the fetus via the placenta. It also delivers wastes product and carbon dioxide from the fetus to the mother’s blood stream so that it may be eliminated. The placenta needs to be firmly implant on the wall of the uterus (endometrium) so that it can maintain contact throughout pregnancy. After delivery, the uterine contractions detach the placenta so that it may be expelled through the birth canal. This detachment ruptures the mother’s endometrial blood vessels and various mechanisms take effect to limit bleeding and seal the vessels.
With a low placenta, these mechanisms may be hampered and can lead to bleeding during and after delivery. This compromises the blood supply to the fetus and also puts the mother’s health at risk due to excessive bleeding from the implantation site. Placenta previa may be marginal (near but not covering the cervical opening), partial (partly covering the opening of the cervix) or complete (totally blocking the opening of the cervix). At times, the term low-lying placenta may be used to describe a placenta that is in the lower half of the uterus yet does not encroach on the cervical opening. It is would therefore not qualify as a marginal placenta previa but can still cause bleeding after delivery.
Causes of Low Placenta
A low placenta is more likely to occur in women with certain risk factors. This, however, does not mean that every woman with one or more risk factors will experience a placenta previa during pregnancy. These risk factors include :
- Multiparity – women who have had many children. This is is increased if there was a short time period between pregnancies or with multiple gestation (twins, triplets and so on).
- Endometrial scarring which may be due to previous surgery involving the uterus, previous pregnancies, cesareans sections, miscarriages, or induced abortions.
- Cigarette smoking, cocaine use.
- Abnormally shaped uterus.
Last updated on September 2, 2018.
