Methemoglobinemia (High Methemoglobin Levels)
What is Methemoglobinemia?
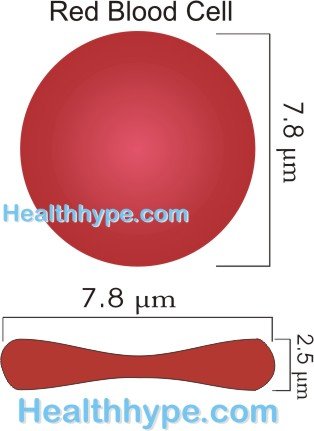
Methemoglobinemia (met-hemo-globin-emia) is a condition where the quantity of methemoglobin in the red blood cells is higher than normal. It is a congenital condition, meaning that it is present from birth, but can develop in life due to exposure to certain toxins. Although methemoglobin is normally present in red blood cells, its quantity is low. Methemoglobin does not carry oxygen unlike hemoglobin. Therefore a rise in the levels of methemoglobin in red blood cells can compromise the ability of these cells to carry oxygen. Very high levels of methemoglobin can be fatal.
What Happens in Methemoglobinemia?
Oxyhemoglobin, usually just referred to as hemoglobin, is the oxygen-carrying component of red blood cells. It is essential for life and a deficiency of oxyhemoglobin is known as anemia. Red blood cells also spontaneously produce another type of hemoglobin known as methemoglobin. It is present in levels below 1% and does not affect the red blood cells normal oxygen-carrying capacity at these levels.
An enzyme known as cytochrome b5 reductase can convert methemoglobin to hemoglobin if necessary. There is also another enzymatic pathway that can convert methemoglobin to hemoglobin but to a lesser degree. These two pathways can ensure that methemoglobin levels are kept in check to a certain degree.
In methemoglobinemia the ability of these pathways to ensure that methemoglobin levels do not rise is compromised. It is the cytochrome b5 reducatase enzyme that is either deficient only in red blood cells or throughout the body that leads to methemoglobinemia.Despite the efforts of the secondary pathway to compensate, it is usually insufficient. Sometimes an abnormality in the hemoglobin molecule also leads to hemoglobinemia.
Ultimately the oxygen-carrying capacity of the blood is compromised and it has a host of effects in the body. The pathological effects depends on the age when the disease starts and the severity of the condition. In the fetus and children (congenital methemoglobinemia), symptoms can affect normal growth and development and ultimately lead to retardation. When the condition arises later in life like during adolescence and adulthood (acquired methemoglobinemia), the symptoms are consistent with anemia since the body’s tissues are starved of oxygen.
Signs and Symptoms
All types of methemoglobinemia cause a bluish discoloration of the skin and mucus membranes (cyanosis) to varying degrees depending on the severity of the conditions.
In congenital methemoglobinemia, infants and children present with delays in developmental milestones, seizures, mental retardation and failure to thrive (FTT) if all cells in the body are deficient of the reductase enzyme (generalized). Dehydration and diarrhea may also be present as a result of acidosis.
With acquired methemoglobinemia that develops later in life, adolescents and adults present with shortness of breath, headaches, fatigue and other symptoms of anemia. The toxins that may cause methemoglobinemia in these causes may also lead to nausea, vomiting and diarrhea. Coma and death is a possibility in severe cases.
Levels of Methemoglobinemia
Normal methemoglobin levels are usually less than 1% but can at times fluctuate between 1% to 2%. It does not cause any problems at these levels. In fact even with the level of methemoglobin rising higher, but less than 10%, there are no symptoms present. It is only once the levels of methemoglobin pass the 10% mark that symptoms become evident since the oxygen-carrying capacity is now significantly compromised. Once these levels pass 70%, death can occur.
10% to 20% methemoglobin
At these levels there is visible discoloration of the skin and mucus membranes, more evident in the inner lining of the mouth and eyes. The skin may appear pale and eventually has a bluish tinge. This is related to the naturally bluish-brown color of methemoglobin and low oxygen levels.
20% to 30% methemoglobin
At these levels the first effects of moderate oxygen deprivation may become evident. It is more noticeable during periods of physical activity and exertion when the body’s demand for oxygen increases. The patient becomes anxious and irritable and complains of headaches.
30% to 50% methemoglobin
At this point there is significantly compromised oxygen availability. A person will experience shortness of breath even at rest and is usually fatigued. Dizziness and confusion may be present, and worsens with any physical activity. The body attempts to compensate by increasing breathing and heart activity, seen as tachypnea and palpitations.
50% to 70% methemoglobin
At these levels the body’s tissues are severely oxygen deprived. The most oxygen-sensitive tissue of the body, the brain, is unable to function normally leading to seizures or progressing to a coma. The heart attempts to pump harder and faster but does not receive sufficient oxygen for its needs leading to an arrhythmia. Elevated carbon dioxide levels in the blood causes acidosis.
Higher than 70% methemoglobin
At these levels, the condition is fatal.
Causes of Methemoglobinemia
The causes determines the type of methemoglobinemia. It can be inherited where genetic defects are passed down from the parent(s) thereby affecting the reductase enzymes or hemoglobin structure. Alternatively, it may arise during the course of life due to exposure to certain toxins.
Inherited methemoglobinemia
- Type 1 congenital methemoglobinemia is due to a deficiency of cytochrome b5 reductase in red blood cells. It is therefore also referred to as erythrocyte reductase deficiency or type Ib5R.
- Type 2 congenital methemoglobinemia is due to a deficiency of cytochrome b5 reductase in all cells. It is also known as generalized reductase deficiency or type IIb5R.
- Hemoglobin M disease is where the hemoglobin structure is abnormal (HbM).
Type 1 and type 2 inherited methemoglobinemia are inherited when both parents pass on the genes to the child (autosomal recessive). The parents themselves usually do not have methemoglobinemia. Hemoglobin M disease arises when just one parent passes the gene to the child (autosomal dominant).
Acquired methemoglobinemia
Acquired methemoglobinemia arises during the course of life. Although it is more frequently seen in adults, it can also affect adolescents, children and infants who are exposed to the causative toxins. It is the more common form of methemoglobinemia. Some of the causative substances that lead to acquired methemoglobinemia includes :
- Nitrates and nitrites that are found in :
– Preservatives
– Fertilizers
– Industrial agents - Fungicides containing copper sulfate.
- Antibiotics such as :
– Dapsone
– Sulfonamides - Anesthetics :
– Benzocaine
– Lidocaine - Analgesics :
– Acetaminophen (paracetamol)
– Celecoxib
– Phenacetin - Antimalarials :
– Chloroquine
– Primaquine - Cancer drugs :
– Cyclophosphamide
– Ifosfamide - Hypnotics :
– Zopiclone
Diagnosis of Methemoglobinemia
Various diagnostic tests can be conducted to confirm methemoglobinemia and evaluate the effects of the condition. Co-oximetry, not pulse oximtery, is the most accurate means of diagnosing methemoglobinemia. It can then be followed up with further tests to diagnose the cause of acquired methemoglobinemia or type of inherited methemoglobinemia. More commonly conducted investigations like an arterial blood gas or pulse oximetry can provide misleading results.
Treatment of Methemoglobinemia
Mild methemoglobinemia may not require any specific treatment for the condition. The causative agent in acquired methemoglobinemia should nevertheless be identified and avoided. Failure to do so can worsen the condition. More severe cases of methemoglobinemia can be treated with the following :
- Methylene blue
- Ascorbic acid (vitamin C)
- Riboflavin (vitamin B2)
Exchange transfusions are reserved for very severe cases. Donor blood is slowly infused while the patient’s blood is simultaneously removed. As an adjunct, hyperbaric oxygen therapy may be considered to increase the oxygen concentration in the patient’s blood.
References