Pancreatic Cysts (Congenital, Neoplastic, Pseudocysts)
What is a pancreatic cyst?
A cyst is an abnormal cavity within an organ that is filled with fluid. It is enclosed by an epithelial membrane that separates it from surrounding tissue. Cysts can occur just about anywhere in the body and may be single or multiple. When it occurs in the pancreas, it is known as a pancreatic cyst. These cysts may be non-neoplastic or neoplastic (benign or malignant). Most cysts are non-neoplastic pseudocysts but some are neoplastic masses. From these neoplasms, some types may be benign (non-cancerous) and others malignant (cancerous). Sometime cysts may be present from birth because it arises from a defect in fetal development and these are known as congenital cysts.
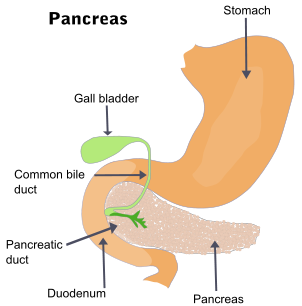
The Pancreas
The pancreas is a multi-function gland that lies in the upper abdomen next to the duodenum of the small intestine. It has both endocrine and exocrine functions. The endocrine activity of the pancreas involves secreting hormones like insulin and glucagon into the bloodstream which regulate the blood glucose levels among other metabolic functions. The exocrine functions largely revolves around digestion. Here pancreatic digestive enzymes are secreted via a duct into the first part of the small intestine known as the duodenum. These enzymes chemically breakdown partially digested food from the stomach so that it can be absorbed into the bloodstream.
True Cyst
A cyst may form when there is some abnormality in tissue proliferation. This can occur in fetal life while the pancreas is still forming or later in life when some factor triggers abnormal growth. Sometimes pancreatic cysts arise along with cysts in other parts of the body – polycystic disease. In these cases it is often associated with genetic diseases as is seen in von Hippel-Lindau disease. The fluid within these cysts are secreted by the epithelial lining that encloses the cavity. True cysts are also known as non-inflammatory cysts.
Congenital Cysts
These cysts are present from birth and arise in fetal life from some abnormality in the development of the pancreatic duct. The size of the cysts can vary from less than a millimeter (mm) to up to 5 centimeters (cm). It is usually surrounded by a very thin outer membrane, however, a fibrous capsule can develop over time if the cyst is filled with excessive amounts of fluid which create a high pressure within yet it does not rupture.
Neoplastic Cysts
A neoplastic cyst or cystic neoplasm develops during life from some abnormality in tissue growth. It may be benign (non-cancerous) or malignant (cancerous). Some may be precancerous meaning that it is benign with the potential to become malignant.
- Serous cystadenomas are benign cysts that tend to occur more frequently in women with advancing age. It is small typically ranging from 1 mm to 3 mm and surgical removal (resection) is usually curative.
- Mucinous cystic neoplasms are also benign cysts but have a potential to become malignant.It occurs almost exclusively in women and most cysts arise in the body or tail of the pancreas. These cysts are generally larger than serous cystadenomas.
- Intraductal papillary mucinous neoplasms (IPMNs) may also be benign or malignant. In contrast to mucinous cystic neoplasms, IPMNs are more often seen in men and tend to involve the head of the pancreas. These cysts tend to involve a large pancreatic duct.
- Solid pseudopapillary neoplasms are a combination solid and cystic mass. The cystic part of the mass is filled with hemorrhagic debris. This type of cyst is more frequently seen in young women. It is a benign mass although some neoplasms may show local aggressiveness similar to a malignancy.
Pseudocysts
A pseudocyst as the name suggests is not a true cyst. It lacks the epithelial lining of a cyst and is filled with digestive enzymes from the pancreas, inflammatory cells and scar tissue. Pseudocysts usually develop after a bout of acute pancreatitis due to trauma, gallstones or with an acute flareup in chronic alcoholic pancreatitis. Almost 75% of all pancreatic cysts are pseudocysts and most will spontaneously resolve. However there is a risk of it becoming infected or compressing adjacent structures in the case of very large cysts.
Most pseudocysts are solitary. It develops when a portion of the pancreas becomes damaged by the action of pancreatic digestive enzymes as is seen in acute pancreatitis. This necrotic tissue often congested with blood is then walled off by fibrous tissue. Inflammatory cells and digestive enzymes may also be trapped within the cyst. The size of these cysts can vary from 2cm to 30cm. Smaller cysts are less likely to cause any symptoms (asymptomatic). It is therefore not uncommon for a person to be unaware of the cyst if it resolves on its own with no complications.
Causes of Pancreatic Cysts
The cause of true cysts are not always known. While some cysts may be associated with a genetic mutation or disorder, it does not always account for all types of neoplastic cysts. Pseudocysts on the other hand are better understood. In children it is more often associated with trauma and gallstones which may also explain its existence in adults. Another likely cause in adults is chronic pancreatitis associated with alcoholism.
Signs and Symptoms
Pancreatic cysts that are less than 2 centimeters are usually asymptomatic. The clinical presentation largely depends on the location and size of the cyst. Some of the more common signs and symptoms include :
- Abdominal pain
- Back pain
- Abdominal mass with/without tenderness
- Nausea and vomiting
Additional symptoms may depend on the compression of surrounding structures by larger cysts. One of the common sites affected by large cysts is the bile duct. Compression of the duct hampers bile excretion and this leads to yellow discoloration of the skin and eyes (jaundice), pale stools and dark urine. Cysts may become infected which presents with severe pain and fever. If a cyst ruptures then it is a medical emergency that needs immediate treatment. A ruptured cyst may also present with reduced consciousness, fainting, bloody vomit (hematemesis) and weak and rapid heartbeat.