Portal Hypertension (High Blood Pressure in Vein to Liver)
Portal Hypertension Definition
Portal hypertension is the medical term for elevated blood pressure with the major vein of the liver, the hepatic portal vein. Although it is most commonly caused by liver cirrhosis, it can be due to a number of other causes that may not even involve the liver. Therefore portal hypertension is an important clinical sign of a wide range of diseases. In the long term, the prolonged hypertension can cause a host of complications within the liver and entire body, some of which can be life threatening.
Portal Hypertension Location
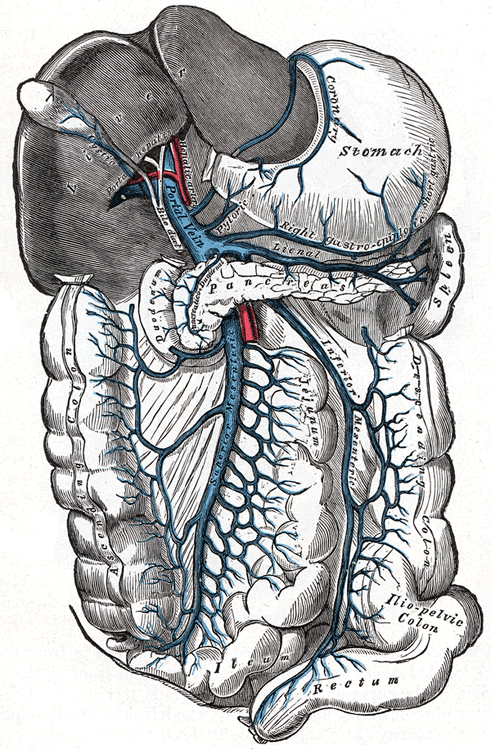
The hepatic portal vein is the major vein that carries blood to the liver. Blood from various parts of the gastrointestinal tract drain into the portal vein. In this way nutrients from the gut can be processed by the liver. Similarly toxins that are absorbed from the gut are first filtered by the liver before the blood empties into the systemic circulation. The portal vein originates behind the pancreas in the right upper quadrant of the abdomen. It measures about 8 centimeters (about 3 inches) in length.
The portal vein also communicates with other veins draining blood from various organs in the pelvis, abdomen and even the thoracic cavity. Blood that filters through the liver then exits through the hepatic veins. It empties into the inferior vena cava which then carries the deoxygenated blood to the right side of the heart.
Picture from Wikimedia Commons
Depending on the nature of the underlying problem and its location, the various causes of portal hypertension can be classified as :
- Prehepatic when the problem lies before the blood reaches the liver.
- Intrahepatic when the problem is located within the liver.
- Posthepatic when the problem lies after the blood flows out of the liver.
Portal Hypertension Pathophysiology
The normal blood pressure within the portal vein is around 5 to 10 mmHg. Blood drains through the liver sinusoids where it filtered by the hepatocytes (liver cells). Portal hypertension is mainly due to an increase in resistance to blood flow or an excess of blood flowing through the vein. For example, in cirrhosis which is the most common cause of portal hypertension, there is increased resistance to blood flow within the liver sinusoids as a result of the tissue damage and swelling.
The elevated blood pressure within the portal vein has several consequences. Firstly blood may be shunted through collaterals leading from other organs. This causes these collateral veins to become engorged. The dilated veins may then rupture leading to bleeding within the abdomen or within the organ. Secondly, in portal hypertension blood can be rerouted through collaterals that communicate with the systemic circulation allowing toxins to bypass filtration in the liver.
Portal Hypertension Symptoms
Portal hypertension on its own does not cause signs and symptoms. The complications of portal hypertension may be symptomatic. Similarly the underlying cause of portal hypertension may be symptomatic.
- Bleeding in the gut which may be sudden and severe :
– Vomiting of blood (hematemesis)
– Black tarry stools (melena) - Fluid accumulation within the abdomen (ascites).
- Enlarged spleen (splenomegaly).
- Brain dysfunction (encephalopathy) marked by difficulty concentrating, poor memory, irritability, problems with sleep and confusion.
- Abdominal pain and sometimes visible veins on the surface of the abdominal wall.
Since portal hypertension is a result of liver diseases like cirrhosis, the following symptoms may also be present in the condition :
- Jaundice
- Nausea and vomiting
- Dark stools
- Pale urine
- Generalized itching (pruritus)
- Bleeding disorders
- Weakness
- Malaise
- Loss of appetite
- Weight loss
Portal Hypertension Causes
The cause of portal hypertension is extensive. Cirrhosis, the most common cause of portal hypertension, is a condition where there is scarring of the liver usually due to chronic liver disease. Some of the common causes of portal hypertension includes viral hepatitis (B and C), alcoholism and non-alcoholic fatty liver disease. There are various other causes of cirrhosis including infections, parasitic infestations, autoimmune diseases, metabolic disorders, iron overload and heavy metal toxicity.
Apart from cirrhosis there are several other causes of portal hypertension, which may not be as common but is nevertheless significant. These causes can be listed by its location – prehepatic (before the liver), intrahepatic (within the liver) and posthepatic (beyond the liver).
Prehepatic Causes
- Blood clot (thrombus) with the portal or splenic vein.
- Abnormal connection between an artery and the portal vein – arteriovenous fistula.
- Tumors that compress the portal vein.
- Very enlarged spleen (massive splenomegaly) due to some other cause which is not a complication of portal hypertension.
Intrahepatic Causes
- Parasitic infection like schistosomiasis (Schistosome worm infection).
- Bile duct destruction (primary biliary cirrhosis).
- Cirrhosis due to any cause.
- Unknown causes (idiopathic portal hypertension).
- Diseases that cause the formation of granulomas, like sarcoidosis and tuberculosis.
- Liver cancer including spread of cancer from elsewhere to the liver (metastasis).
- Cysts in the liver with diseases like polycystic liver disease.
Posthepatic Causes
- Blockage in the hepatic veins exiting the liver.
- Obstruction within the inferior vena cava (IVC).
- Various heart diseases that causes a backing up of blood leaving the liver :
– Right-sided heart failure.
– Constrictive pericarditis.
– Tricuspid regurgitation.
– Restrictive cardiomyopathy.
Portal Hypertension Diagnosis
Portal hypertension is usually diagnosed after a clinical evaluation where the complications can be identified, coupled with a medical history indicating a possible cause. Although there are procedures to directly measure the pressure within the portal vein, these procedures are invasive and therefore not routinely conducted when portal hypertension is suspected. Instead other investigations are conducted to identify a possible cause, assess the blood flow through the portal vein and isolate complications associated with portal hypertension. These investigations include :
- Ultrasound
- Computed tomography (CT) scan
- Magnetic resonance imaging (MRI) angiography
- Endoscopy
Portal Hypertension Treatment
The treatment for portal hypertension should be directed at the cause and any complications that may have arisen should also be treated. Ruptured varices is one of the main reasons that portal hypertension is diagnosed. The bleeding needs to be attended to immediately when it is very profuse. Even if varices have not as yet ruptured, treatment should still be undertaken to reduce the chance of a rupture in the future. The following measures are :
- Endoscopic treatment for upper gastrointestinal varices include banding or sclerotherapy. Repeat endoscopy needs to be conducted at regular intervals to asses the condition and identify any new varices.
- Medication is used to reduce pressure within the varices and portal vein. These drugs include :
– propanolol
– nadolol
– vasopressin
– nitroglycerin
– isosorbide mononitrate
In the event that these measures are not able to yield the desired results and treating the cause is not successful, other treatment options need to be considered. The two procedures that may be conducted includes a transjugular intrahepatic portosystemic shunt (TIPS), where a stent is placed in the liver, or a distal splenorenal shunt (DSRS) where the splenic and left kidney veins are connected to reduce pressure.
References :
my.clevelandclinic.org/disorders/portal_hypertension/hic_portal_hypertension.aspx