Retinitis Pigmentosa Causes, Symptoms, Treatment
There are many eye conditions that can lead to loss of vision, either partial or complete. Cataracts and macular degeneration are two relatively common eye disorders that lead to impaired vision. Another condition is retinitis pigmentosa which is rare but nevertheless a cause of blindness.
What is retinitis pigmentosa?
Retinitis pigmentosa is a group of disorders where the light-sensitive inner lining of the eye, retina, breaks down. It is a genetic disorder that is inherited. There is gradual loss of peripheral vision and difficulty with night vision. Eventually it leads to blindness. Retinitis pigmentosa affects about 1 in 4,000 people. Depending whether the genes associated with retinitis pigmentosa is dominant or recessive, it can appear in the forties or as early as the twenties. However, it can even arise in infancy.
There is currently no cure for retinitis pigmentosa. Prosthetics and implants may help to recover some vision while certain treatments like electrical stimulation therapy can preserve some vision in the early and intermediate stages of retinitis pigmentosa. Certain supplements and drugs may slow down the progression of the disease to some extent but not all have been conclusively proven to be effective in clinical trials. Despite being a rare condition, about 1% of the population carries genes that predispose them to retinitis pigmentosa.
Causes of Retinitis Pigmentosa
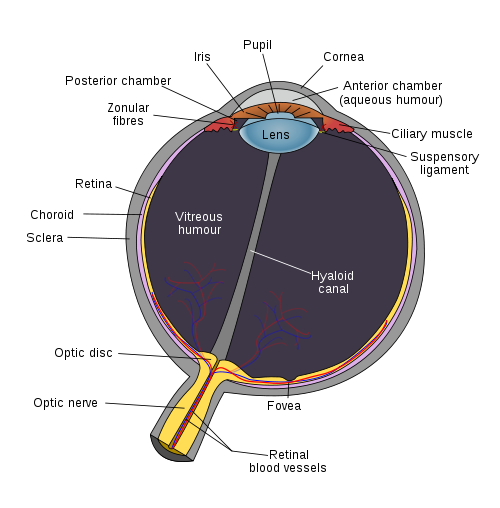
The retina is the inner lining of the eye which responds to light that strikes it. This light-sensitive layer elicits electrical impulses in response to light which then travels through nerves to the brain. These electrical signals are deciphered by the visual centers in the brain and gives rise to the sense of vision. Certain areas of the retina, like the macula, have the highest concentration of the specialized photoreceptors responsible for vision, known as the rods and cones. Therefore light striking this region will give the clearest vision.
The retinal pigment epithelium (RPE) is one of the structures in the eye that is affected in retinitis pigmentosa, along with the photoreceptors – rods and cones. The genetic defects in retinitis pigmentosa causes these structures to die (apoptosis). The rods are predominantly affected. First the rods shorten and then eventually die, more so towards the mid periphery of the retina. This cell death of rods leads to vision loss. Cone cell death occurs in a similar way. However, it usually occurs later in retinitis pigmentosa.
Dominant and Recessive
There are some 32 genes that pass on the traits associated with retinitis pigmentosa. When it is dominant then it is more likely to be passed from parent to child. This is usually associated with retinitis pigmentosa in the forties. Sometimes the trait may be recessive and the gene has been passed down from generations before. In other words it can suddenly appear in a person despite no immediate family members having it. This is usually associated with earlier onset retinitis pigmentosa like in the twenties.
It is important to note that carrying these genes will not necessarily mean that a person will develop retinitis pigmentosa. About 1 in 100 people are carriers of these genes yet it only affects about 1 in 4,000 people. Although genetics is known to be the main factor in retinitis pigmentosa, the reason why it occurs in some carriers and not others is not always clear. It is believed that with certain genes present, stress light exposure may play some role in the development of retinitis pigmentosa.
Signs and Symptoms
The symptoms of retinitis pigmentosa is similar to many other more common eye conditions where there is vision loss. Therefore it is important that an eye specialist is consulted in order for the correct condition to be diagnosed. The signs and symptoms of retinitis pigmentosa includes:
- Poor night vision
- Narrowing of the field of vision (loss of peripheral vision)
- Flashes of light (photospia)
Most of the other clinical findings are made by a medical professional during examination of the retina. It is important to note that these symptoms can start as early in childhood with infantile-onset retinitis pigmentosa. The child, as is the case with the adult with retinitis pigmentosa) can have normal visual acuity. About 50% of patients with retinitis pigmentosa will develop a type of cataract known as a subcapsular cataract. Correcting the cataract will not treat the retinitis pigmentosa.
Diagnosis of Retinitis Pigmentosa
Retinitis pigmentosa has to be diagnosed by an eye care professional. It is not uncommon for the symptoms to be first associated with age-related macula degeneration which is the leading cause of senior blindness. However, macular degeneration and retinitis pigmentosa are two different conditions. Sometimes people mistake retinitis pigmentosa symptoms for a cataract. While a posterior subcapsular cataract can occur in up to 50% of retinitis pigmentosa patients, it as well is a separate condition.
Comparatively retinitis pigmentosa is much rarer than these other macular degeneration or cataracts. Drug toxicity may also be suspected as well as certain infections which could cause similar symptoms. These conditions need to be excluded during diagnosis. A number of tests may be conducted, with the most important being an electroretinography (ERG). Sometimes an electro-oculogram (EOG) may also be done as well as color testing, dark adaptation and genetic testing to confirm a diagnosis of retinitis pigmentosa.
Treatment of Retinitis Pigmentosa
There is no cure for retinitis pigmentosa at this point in time. There is also no conclusive indication that preventative measures may work for retinitis pigmentosa although practitioners may recommend a diet rich in fruits and vegetables, especially leafy green vegetables. In addition non-toxic doses of certain vitamins and minerals may be recommended. Light stress may have some role to play in the development of retinitis pigmentosa and it is therefore recommended that UV protective eye wear be used.
Medication
Medical treatment, both clinically verified and those still undergoing research, includes:
- Vitamin A/beta carotene, lutein/zeaxanthin and docosahexaenoic acid (DHA) supplementation.
- Acetazolamide
- Calcium channel blockers
- Valproic acid
It is important to note that not all these supplements and drugs may be beneficial. Furthermore these treatment measures cannot reverse the condition but may play some role in slowing its progression.
Surgery
Surgical treatment includes:
- Retinal pigment epithelium (RPE) cell transplantation
- Retinal prosthesis
- Retina implant
- Gene therapy (experimental)
References: