Sporotrichosis (Sporothrix Fungal Infection) Information and Pictures
What is sporotrichosis?
Sporotrichosis is an infection with a soil fungus. Unlike dermatophyte (skin fungus) infections such as tinea pedis (athlete’s foot), it is not limited to the outermost layers of the skin. Instead it can penetrate into the deeper tissue involving the joints, bones and rarely even the lungs. Infection of multiple organs is uncommon but can occur in immune deficient states such as with AIDS. Sporothrix infection of the skin can be easily treated but treatment of deeper infections can be difficult. The diagnosis is often missed since sporotrichosis is not a common infection although the fungus exists across the globe.
Sporothrix Infection
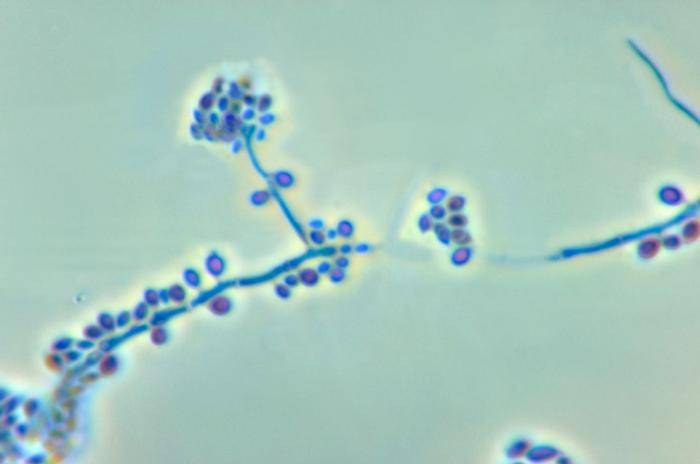
Sporotrichosis is caused by the fungus Sporothrix schenckii. It is a dimorphic fungus meaning that it can exist as a mold or yeast. This occurs with differences in temperature – about 25 degrees Celsius in the mycelial form and 37 degrees Celsius as an yeast. Sporothrix schenckii is found on plants and tree bark as well as plant debris in the soil. It can also be transmitted to humans by infected cats, through animal bites especially tree dwelling wild animals like squirrels and insect stings.
The fungus invades the skin and underlying tissues through a break in the skin. Initially it starts as a skin infection – cutaneous sporotrichosis. By spreading through the lymphatics (lymphocutaneous sporotrichosis) it travels through the system to multiple sites. It may also extend to neighboring tissue and can even reach distant organs through the bloodstream (hematogenous spread) which is uncommon. Once it reaches deeper tissue it is referred to as extra-cutaneous spirotrichosis. Involvement of the bones and joints is known as osteoarticular sporotrichosis. In rare cases it may be inhaled to cause an infection in the lung (pulmonary sporotrichosis) or it is sometimes ingested. Spread through the bloodstream to infect the meninges, the linings around the brain and spinal cord, is uncommon and mainly seen in HIV/AIDS patients. This is known as meningeal sporotrichosis. The fungus can spread throughout the body to infect multiple organs simultaneously and is then known as disseminated sporotrichosis.
Causes of Sporotrichosis
In order to cause an infection, the sporothrix fungus has to penetrate the outer layers of the skin. It can be acquired from contact with :
- Plants
- Trees
- Soil
- Thorns
- Pine needles
- Barbs and wire
- Infected animals like cats and horses
- Animal bites
- Insect stings
Therefore sporotrichosis is more likely to be seen in the following individuals :
- Farm workers
- Gardeners
- Landscapers
- Nursery workers
- Tree fellers
- Loggers
- Carpenters
However, any person can develop sporotrichosis through secondary contact. Although the Spirothrix fungus has a worldwide, certain areas like northeast China is considered to be endemic.
Sporotrichosis and HIV/AIDS
HIV infection and AIDS have also played a role in the rise of this uncommon fungal infection in recent years. After the initial inoculation at the site of the broken skin, the fungus can quickly spread with limited host defenses. Therefore very rare extra-cutaneous manifestations such as sporothrix meningitis is mainly seen in HIV/AIDS patients where spread through the bloodstream is more likely to occur. Disseminated disease is almost exclusively seen in HIV/AIDS.
Sporotrichosis Symptoms
The signs and symptoms of sporotrichosis depends on the affected region. Fever and other signs of systemic disease are usually absent.
Skin
In most people sporotrichosis is limited to the skin (cutaneous) and spreads along the lymphatic channels (lymphocutaneous). Sometimes it is isolated just to the skin (non-lymphatic sporotrichosis). It is usually limited to the upper limbs as inoculation tends to occur in the hands and extend to the arms. Typically the person is without a fever and there is no signs of the infection spreading to the deeper tissue.
The skin lesions appear :
- About 3 weeks after the injury but can be as soon as 1 week or as delayed as 10 weeks after.
- As a nodule under the skin (subcutaneous) at the site of inoculation which then ulcerates (open sore).
- With swollen lymph nodes (lymphadenopathy) and additional skin lesions along the route of the lymphatic channel (satellite lesions).
- Milder cases of non-lymphatic sporotrichosis appears as a red, thickened and scaly rash while more severe cases may result in ulcers (open sores). However, there are no satellite lesions.
Skin lesions may or may not occur with disseminated disease where multiple other organs are involved.
Bones and joints
Osteoarticular sporotrichosis is the term when the bones and joints are infected with the Sporothrix fungus. It is often mistaken for rheumatoid arthritis and can persist for up to years before it is accurately diagnosed. The joints are swollen and painful. Bone is gradually destroyed over years. Depending on the duration and severity, there may be a significant degree of immobility of the affected joint. Although one joint is usually involved, the spread of the infection may also affect other joints in the long term.
Lungs
Pulmonary sporotrichosis is transmitted through inhalation and is more likely to occur in immune compromised states especially HIV/AIDS. The condition usually develops over months or years and presents as pneumonia. There is evidence of chronic obstructive pulmonary disease (COPD) in long term cases. In most cases, the only symptom is a persistent cough.
Other organs
Disseminated sporotrichosis is where the infection spreads throughout the body affecting multiple organs and at times at different sites. It is a rare form of sporotrichosis and more likely to occur in immune compromised states. Apart from lymphatic spread and direct infiltration to surrounding organs, the fungus may spread via the bloodstream (hematogenous) to reach various sites throughout the body. Organs that may be affected includes :
- Eye
- Larynx
- Meninges
- Mouth
- Paranasal sinuses
- Prostate (men)
Pictures
The cutaneous sporotrichosis pictures below are from Dermatology Atlas Brazil (atlasdermatologico.com.br). It is not suitable for sensitive viewers.
Sporotrichosis Treatment
Sporotrichosis needs to be treated with antifungals. The preferred antifungal drug is itraconazole.
- Skin : itraconazole, terbinafine, saturated solution of potassium iodide (SSKI)
- Bones and joints : amphotericin, itraconazole
- Lung : amphotericin, itraconazole
- Meninges : amphotericin, itraconazole, potassium iodide (SSKI)
- Disseminated : amphotericin, itraconazole
Surgical removal of the severely damaged parts of the bones and lungs may be necessary. An alternative approach for cutaneous sporotrichosis in pregnant women is heat therapy since azoles cannot be used. Amphotericin B may have to be used if this therapy is not effective.
References
1. Sporotrichosis. Emedicine Medscape
2. Sporotrichosis. DermNet NZ