Supraventricular Tachycardia (SVT)
Supraventricular Tachycardia Definition
Supraventricular tachycardia (SVT) is a condition where there heart beats rapidly (tachycardia) due to electrical impulses originating the region above the heart’s ventricles, the chambers that push blood of the heart. It is also known as paroxysmal supraventricular tachycardia (PSVT). The condition is typically episodic meaning that it does not occur all the time. These episodes start and end very suddenly. A heart rate faster than 100 beats per minute (compared to the normal 60 to 90 beats/minute) is considered to be tachycardia.
Supraventricular Tachycardia Types
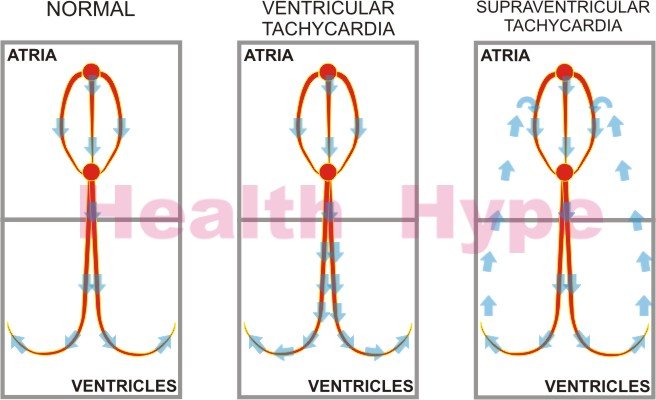
Supraventricular tachycardia can affect people of all age groups. It may be asymptomatic in some patients. Other affected individuals may show moderate to severe symptoms. Depending on the place of origin of the electrical impulse that causes rapid heartbeats, supraventricular tachycardia may be classified as an atrial (originating from atrium) or atrioventricular (originating from atrioventricular or AV node) tachyarrhythmia.
- Atrial tachyarrhythmias may include tachycardias related to sinus and atria.
- AV tachyarrhythmias may include tachycardias related to atrioventricular node.
Supraventricular Tachycardia Incidence
Nearly 3 in every 1,000 persons develop supraventricular tachycardia. Females and older people are at a greater risk. Supraventricular tachycardia is more frequent in people who suffer from heart attacks, defects in the valve, rheumatic heart disease, inflammation of the lining surrounding the heart (pericarditis), chronic lung disease, pneumonia, alcoholism, and digoxin toxicity.
Supraventricular Tachycardia Pathophysiology
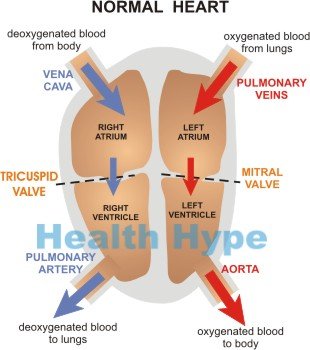
Normal Heart Beat
The human heart is made up of two chambers (atria) that receive blood and two chambers (ventricles) that push out blood. The atria sit above the ventricles.The blood enters the heart through the upper atrial chambers. Electrical impulses generated from a region known as the sinoatrial (SA) node located in the upper region of the heart spreads to all the chambers of the heart and makes the muscular walls contract.
The atria chambers contract first and blood is pushed into the ventricles. The ventricles then contract and blood is pushed out of the heart. One heartbeat is made up of a sequence of atrial and ventricular contraction. In this way blood is received by the heart (atria), sent to the ventricles and the forced out of the heart to the lungs (from the right ventricle) or to the rest of the body (from the left ventricle).
Control of Heart Beat
Factors that influence the rate of heart contraction include :
- hormones like adrenalin
- oxygen demand
- nerve impulses
A problem with any of these factors can result in abnormal heartbeat rhythms (dysrhythmia or arrhythmia).
In supraventricular tachycardia, abnormally fast electrical impulses are generated in the atria. This causes the heart to beat very fast and the heart muscles are not able to relax properly between contractions. Subsequently the heart chambers are not able to contract strongly as they never recover fully from the previous contraction. They also do not fill up with adequate blood. Due to these reasons, the efficiency of blood supply to the rest of the body is diminished.
Supraventricular Tachycardia Symptoms
Symptoms of supraventricular tachycardia vary, depending on an individual’s overall health. People suffering from heart damage and other medical problems are more likely to demonstrate symptoms of supraventricular tachycardia. Reduced oxygen supply due to compromised cardiac output tends to cause the first symptoms in the brain, which is the most oxygen sensitive organ in the body.
The following symptoms are seen in people suffering from supraventricular tachycardia :
- Palpitations (forceful pounding of heart)
- Dizziness, lightheadedness, or fainting
- Fatigue
- Breathlessness
- Anxiety, sweating and nausea
- Chest pain or tightness
- Infants – irritability, sweating, reduced appetite, discolored skin, and pulse rate of 200 to 250 beats per minute.
Symptoms appear suddenly and may last from a few seconds to days. It often disappears on its own. Due to rapid beating, the heart becomes less effective in pumping enough blood to various organs in the body. This affects the normal functioning of other organs which in turn causes other symptoms.
Supraventricular Tachycardia Complications
Supraventricular tachycardia patients have a small risk of sudden death. Complications usually arise because of underlying heart diseases. Patients without any structural abnormalities in the heart rarely show severe complications. In patients with weak hearts, supraventricular tachycardia can result in a heart attack, heart failure, fluid accumulation in the lungs, heart pain, unconsciousness, and heart muscle disease.
Supraventricular Tachycardia Causes
SVT may be associated with the following medical conditions:
- Heart failure
- Hardening of the arteries (atherosclerosis)
- Diseases like chronic lung disease, thyroid dysfunction, pneumonia
- Pulmonary emboli (blood clots in the lung)
- Inflammation of the lining of the heart
- Drug abuse like cocaine
- Alcoholism and smoking
- Excessive caffeine intake in tea, coffee, or soft drinks
- Pregnancy
- Emotional stress
- Structural abnormalities in the heart, Wolff-Parkinson-White (WPW) syndrome (characterized by extra electrical tissue, which sets up abnormal electrical circuits)
- Side effect of medications (e.g., digitalis, cold remedies, or asthma medications)
Risk factors
Digoxin toxicity and structural defects in the heart increase the risk of supraventricular tachycardia.
Supraventricular Tachycardia Diagnosis
The following tests are conducted to diagnose supraventricular tachycardia:
- Laboratory tests determine electrolyte levels, complete blood count, thyroid levels, and digoxin levels.
- Chest radiography determines the presence of fluid in lungs, pneumonia and heart defects.
- Magnetic resonance imaging (MRI) of the heart is a useful diagnostic tool in case of congenital heart diseases.
- The painless, quick and non-invasive electrocardiogram (ECG) test detects the electrical activity of the heart.
- Ambulatory ECG monitors the heart activity over 1 to 2 days.
- The non-invasive ultrasound echocardiogram (ECHO) shows images (sonograms) of the heart walls, valves, muscles and the left ventricle.
- In stress test, an ECG is done both when the heart is at rest and while it is under stress. It diagnoses coronary heart diseases and other heart-related problems (ischemia).
- Coronary angiographies and cardiac catheterizations are done in rare cases of severe symptoms like significant risk for coronary artery disease.
Supraventricular Tachycardia Treatment
Treatment is aimed at reducing the heart rate and breaking the electrical circuits form due to abnormal conducting pathways.
Electrical interventions
Immediate treatment is needed for unstable patients with chest pain, low blood pressure, or a failing heart that shows fast heartbeats. Cardioversion (electrical shock) restores the normal rhythm of the heart. Synchronized cardioversion is performed on unstable or deteriorating patients.
Physical interventions
Vagal maneuvers involve coughing, holding breath, dipping face in cold water, and tensing stomach muscles. These exercises tone the vagus nerve of the heart, which releases substances that decrease heartbeats. This procedure stops SVT in many cases by breaking the abnormal electrical circuits.
Carotid massage of carotid artery in the neck slows the heart rate in young patients.
Medications
- IV administration of adenosine blocks the SA node conduction briefly and decreases the heart rate in the majority of patients. Side effects include transient chest pain, facial flushing, nausea, breathlessness, and dizziness. In case of adenosine-resistant patients, digoxin, calcium channel blockers (verapamil and diltiazem), or beta-blockers (metoprolol or esmolol) are used.
- Intravenous administration of propafenone, procainamide, or flecainide is recommended for stable patients.
- Amiodarone is given to patients with impaired functioning of the left ventricle, structural heart diseases, or heart failure.
- Medical implants are sometimes used. Example a pacemaker implanted inside the heart works as the SA node.
Radiofrequency Catheter Ablation
Catheter ablation is frequently performed for treating SVTs. A catheter is directed to the heart where the nerve carrying the abnormal impulse is cauterized with radiofrequency energy.
Supraventricular Tachycardia Lifestyle
- Dietary changes like eating low-fat, low-cholesterol, and low-salt diet with more vegetables prove helpful.
- Alcohol, smoking, caffeine intake, and illicit drug use should be avoided.
- Regular exercise lowers the heart rate and the blood pressure and makes the heart stronger and efficient in pumping blood.
- Relaxation techniques (like deep breathing, muscle relaxation, biofeedback, and meditation) help in managing stress.
- Maintaining a healthy body weight is helpful.
References :
http://www.webmd.com/heart-disease/tc/supraventricular-tachycardia-overview
http://emedicine.medscape.com/article/156670-overview
http://www.patient.co.uk/doctor/Paroxysmal-Supraventricular-Tachycardias.htm