Inflammatory Bowel Disease (IBD) Types, Causes, Symptoms, Treatments
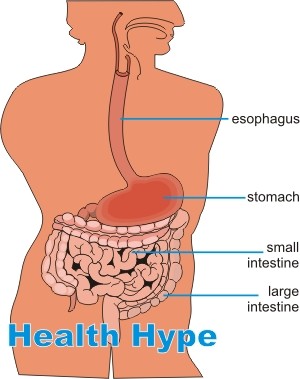
The alimentary tract extends from the mouth to the anus. Most of the length of this tract is made up on the bowels, namely the small intestine and large intestine. The small intestine is divided into three parts – duodenum (leading from the stomach), jejunum and ileum (leading to the large intestine). The large intestine is composed of the cecum, colon and rectum.
Most of the digestion, absorption and stool formation occurs within the bowels. Various chronic diseases can afflict the bowels. One of the more common of these conditions is inflammatory bowel disease or IBD. This condition should not be confused with inflammatory bowel syndrome (IBS) which is a functional disorder of the bowels, meaning that it is in a state of dysfunction although there is not evident pathology of the bowels.
What is inflammatory bowel disease?
Inflammatory bowel disease (IBD) is a a chronic disease characterized by varying degrees of inflammation of mainly the bowel but may extend to other parts of the gastrointestinal tract. There are two main types of IBD – Crohn’s disease and ulcerative colitis. Although there are several key differences between the two conditions, the clinical presentation is largely the same and may be difficult to differentiate. Crohn’s disease more frequently affects the ileum and colon but can occur in any part of the alimentary tract. Ulcerative colitis is only seen in the colon and rectum.
Both Crohn’s disease and ulcerative colitis appear to be due to the same mechanism, the cause of which is largely unknown. Inflammatory bowel disease afflicts some 1 to 2 million Americans with most cases being diagnosed in early adulthood, although it may be very infrequently seen in children. Ulcerative colitis is more common but only marginally so and women are more prone than men to developing IBD.
Pathophysiology of IBD
As previously stated, the cause of inflammatory bowel disease is unknown (idiopathic). It appears to be due to a defective mucosal immune mechanism, however, inflammatory bowel disease is not considered as an autoimmune disease as such. Instead it is believed that a combination of the following mechanisms may be responsible for the chronic inflammation :
- defective host response to the normal intestinal flora (naturally-occurring bowel bacteria).
- dysfunction of the epithelium of the intestine.
- abnormal mucosal immune responses.
These defects are largely due to a genetic predisposition and may therefore be seen in families although this is not always the case.
Intestinal Bacteria
The bowels contain trillions of bacterial cells which play an important role in digestion and absorption of various nutrients. These naturally-occurring bacteria, known as the normal intestinal flora, also help to prevent the invasion of the bowel by foreign pathogens. However, the population of these bacteria needs to be closely controlled by various mechanisms within its microenvironment to prevent it from becoming harmful to the bowels.
There is some evidence to suggest that in inflammatory bowel disease, the body forms antibodies against these bacteria which then leads to inflammation that is ongoing as the bacteria are constantly replenished. The bacterial population may also, for some reason or the other, pass beyond its normal acceptable limits in inflammatory bowel disease.
Epithelial Tight Junction Barrier
The neighboring cells that make up the mucosal epithelium lie closely together and practically join together to form an impermeable membrane. This close association is known as a tight junction and the effect of the epithelial barrier is to ensure that substances within the epithelial tissue does not leak out into the gut and at the same time substances do not enter the tissue spaces without being absorbed, either passively or actively, as required.
One of the hypotheses around the pathogenesis of inflammatory bowel disease suggests that this epithelial tight junction barrier function is compromised to some degree and this may allow for unregulated transport of substances across the mucosal epithelium. Ultimately this triggers inflammation of the bowel wall. A defective transport of substances across the epithelial lining may also be another factor in inflammatory bowel disease, irrespective of the integrity of the tight junction barrier.
Mucosal Immune Response
Mucosal epithelium lines the gastrointestinal tract from the mouth to the anus. Although there may be differences in the lining of the various portions of the gut, it is largely the same structure. The mucosa is not a tight impermeable barrier like the skin but is often just as exposed to the environment – air, foods and drinks. It has its own immune response known as the mucosal immune system which is geared to protect it from any invading pathogens.
In this manner it also prevents infiltration into deeper tissue and infection from spreading to the rest of the body. In inflammatory bowel disease this mucosal immune response appears to be defective. Inflammatory mediators are abnormally activated and inflammation therefore sets in despite the obvious absence of any threat to the mucosal epithelium.

Causes of Inflammatory Bowel Disease
Although the exact cause has not as yet been identified despite a better understanding of the mechanism in recent years, it is believed that some external factor triggers the process in a person who is genetically susceptible. Trigger factors that have been suggested include a previous infection (possibly infectious gastroenteritis), exposure to cow’s milk or other animal protein and underlying autoimmune diseases, not specifically affecting on the bowel, like autoimmune thyroiditis and systemic lupus erythematosus (SLE). Cigarette smoking appears to play some role in inflammatory bowel disease but the exact interaction is not clear as yet. Appendectomy, removal of the appendix, appears to play a protective role which is also not clearly understood as yet.
Crohn’s Disease vs Ulcerative Colitis
The main differences between Crohn’s disease and ulcerative colitis are listed below. Other differences and similarities relating to ethnicity, recurrence after surgery, cancer potential, nutrient malabsorption and cigarette smoking are discussed further under the respective conditions.
Location
The anatomical distribution is as follows :
- Crohn’s disease : Affects any part of the gut, from the mouth to the anus, but mainly the ileum (last part of the small intestine) and colon.
- Ulcerative colitis : Only occurs in the colon and rectum.
Lesions
The type of lesions is as follows :
- Crohn’s disease : Skip lesions with inflammation extending through the entire wall of the bowel (transmural). Fibrosis is significant.
- Ulcerative colitis : Diffuse inflammation isolated to the mucosa and submucosa. Little or no fibrosis is seen.
Ulcers
Ulcers occur in both conditions but may vary in size and depth as follows :
- Crohn’s disease : Deep narrow ulcers, fissures and fistulas.
- Ulcerative colitis : Large, shallow ulcers.
Signs and Symptoms of IBD
The signs and symptoms of inflammatory bowel disease is similar to many other infectious and inflammatory conditions of the lower digestive system. Due to the similar presentation, IBD may often be confused with IBS. However, inflammatory bowel disease and irritable bowel syndrome are two separate conditions.
Diarrhea
Recurrent or persistent diarrhea is the main feature of both Crohn’s disease and ulcerative colitis. In Crohn’s disease this is watery, large volume diarrhea with no blood or mucus. In ulcerative colitis, bloody diarrhea is a cardinal sign, along with mucus in patients with proctitis. Some ulcerative colitis patients may experience frequent bowel movements with small-volume loose stools and rarely may even experience constipation with hard stools between acute attacks.
Abdominal Pain
Abdominal pain is significant in Crohn’s disease which intensifies with eating and passing stool. In ulcerative colitis, abdominal pain is not as prominent although there is some abdominal discomfort and cramping which is often temporarily relieved by defecation. In severe cases of ulcerative colitis, however, the pain is intense and not ameliorated by bowel movements.
Weight Loss
Weight loss is prominent in most patients with Crohn’s disease partly due to pain associated with eating and malabsorption. Ulcerative colitis patients are largely unaffected with regards to weight loss except in very severe cases although there may be some temporary loss of weight during acute attacks.
Other Features
- Anemia
- Anorexia
- Arthralgia (joint pains)
- Eye inflammation (uveitis)
- Fever
- Lethargy
- Malaise
- Mouth sores
- Skin disorders
Treatments for Inflammatory Bowel Disease
Inflammatory bowel disease is a difficult condition to treat and manage and both surgical and medical treatment (the use of medication) is primarily directed at reducing the severity of symptoms during active phases and decreasing the frequency of these flareups. Treatment, both medical and surgical, should be incorporated with dietary and lifestyle changes, although diet modification is of limited value in inflammatory bowel disease.
Medications for Inflammatory Bowel Disease
Medical treatment is determined by the clinical presentation at the time. Acute flareups require symptomatic treatment although this has to be limited in severe acute phases. Therapy during remission may be directed at preventing an acute flareup or even managing the odd mild persistent symptom.
Acute Flareups in IBD
Symptomatic treatment will depend on the use of one or more of these drugs depending on the clinical presentation at the time :
- Antidiarrheals such as loperamide or combination dipheoxylate and atropine for controlling diarrhea, reducing frequency of bowel movements and urging. Methylcellulose or psyllium powder may also be effective for mild diarrhea.
- Antispasmodics such as dicyclomine to relieve intestinal cramping.
- Pain relievers such as acetaminophen may be effective for mild pain but aspirin, ibuprofen and narcotics should be avoided particularly in the long term.
The use of these medications in a severe acute flareup can exacerbate the condition and lead to complications. In-hospital management may be the preferred option in these instances. Many of the drugs discussed below under step-wise medical treatment is useful for acute flareups, inducing remission and maintaining remission (long term management).
Step-Wise Medical Treatment
Long term management is intended to prevent flareups or at least reduce the frequency and severity. In terms of medication, a step-wise approach to therapy is employed where the next step is commenced once the patient fails to respond to the current regimen.
Step 1 – Aminosalicylates and Antibiotics
Aminosalicylates are derivatives of 5-aminosalicylic acid that are used as for its anti-inflammatory action in both treating flareups and maintaining the disease in remission. The different types of aminosalicylates used includes :
- Sulfasalazine
- Mesalamine
- Balsalazide
- Olsalazine
All of these aminosalicylates appear to be equally effective and a better response to these drugs is noted in ulcerative colitis with Crohn’s disease. It is more effective to prevent recurrence after surgery in Crohn’s disease. Aminosalicylates may be administered orally or rectally (enema or suppository).
Antibiotics are more frequently used in Crohn’s disease as it is more likely to cause antibiotic-associated colitis in ulcerative colitis. Nevertheless, it is used sparingly in ulcerative colitis, particularly prior to surgery. Antibiotics have been shown to induce remission in inflammatory bowel disease (IBD). The more commonly used antibiotics are :
- Metronidazole
- Ciprofloxacin
Step 2 – Corticosteroids
Corticosteroids are anti-inflammatory drugs that are useful in acute flareups and for inducing remission but not for maintaining remission. These drugs should not be used long term due to the host of side effects, many of which are serious and severe. It is, however, not uncommon for some patients to experience an acute exacerbation of the condition upon discontinuing corticosteroids if the condition has not slipped into remission before drug cessation. Corticosteroids can be administered orally, topically or intravenously with the latter being preferred in the hospital setting for its rapid action and better control of dosing.
Step 3 – Immune Modifiers and TNF Inhibitors
Immune modifiers are drugs that typically suppress the immune system thereby reducing the inflammation. These drugs may affect the white blood cell count. It is useful for both inducing and maintaining remission and so it should be used only after other measures, particularly aminosalicylates, fail to act or cannot be tolerated. Immune modifiers may also be useful in reducing dependence on corticosteroids particularly in long term management where corticosteroids should not be used for maintaining remission. These type of drugs include :
- 6-mercaptopurine (6-MP)
- Azathioprine
TNF inhibitors, also known as anti-TNF drugs or anti-TNF-alpha monoclonal antibodies, also counteract immune action by binding and neutralizing tumor necrosis factor (TNF) that is secreted by white blood cells. TNF mediates tissue damage. These drugs are more effective for Crohn’s disease but is also used in ulcerative colitis. As with immune modifiers, it has severe side effects and is not the first line of treatment. The anti-TNF agents used for IBD include :
- Infliximab
- Adalimumab
- Certolizumab pegol
Another type of monoclonal antibody known as natalizumab acts by blocking integrin, the molecule that contributes to lymphocyte accumulation in the bowels. It is useful for Crohn’s disease but not routinely used as a step III measure because TNF inhibitors are usually more effective.
Surgery for Inflammatory Bowel Disease
Surgery is considered when medical treatment (medication) fails to act. It is curative for ulcerative colitis and therefore indicated for management where medication is ineffective. Surgery for Crohn’s disease should only be considered when the complications of IBD arises.
For ulcerative colitis, surgery may involve proctocolectomy (removal of rectum and part/entire colon). A stoma (ileostomy) is necessary to allow waste material to pass out of the small intestine (terminal end known as the ileum) and into the exterior. Another procedure that may be considered for ulcerative colitis is colectomy (surgical removal of colon) with ileoanal pouch (ileoanal anastomosis). An ileoanal anastomosis connects the terminal part of the small intestine (ileum) to the anus but a pouch is formed with the small intestine to serve as a reservoir for feces.
Since Crohn’s disease can affect any part of the alimentary tract, surgery does not have the same results as is the case with ulcerative colitis. Segmental resection of the portion of the tract that is most effective is not curative and recurrence rates may be as high as 50%. Anastomosis is necessary and this may involve the ileum to the rectum (ileorectal anastomosis) or healthy ileum to colon (ileocolonic anastomosis). Despite surgery not being curative with Crohn’s disease, patients may respond better to medication for maintaining remission after surgery.