What is Cervical Cancer? Location, Pre-Cancerous, Growth Patterns
Cervical cancer is cancer that develops in the cervix – the narrow, lower part of the uterus which leads into the vagina. It is often asymptomatic in the early stages. Symptoms such as abnormal vaginal bleeding, pelvic pain, and pain during sexual intercourse usually appear late, similar to uterine cancer (endometrial) and vaginal cancer. Although it may occur at any age, middle aged and older women are most commonly affected.
The pre-cancerous stage (carcinoma in situ) or early stage cervical cancer can be detected by a pap smear. Routine testing is therefore advisable for all girls and women, especially those who are sexually active. Infection with human papillomavirus (HPV), which is transmitted through sexual contact, is a very important risk factor associated with the development of cervical cancer. Vaccination against HPV and early detection of the cancer by routine pap test can significantly lower the incidence of cervical cancer and increase the chance of successful treatment. Although the incidence of cervical cancer has decreased in the United States over the past few years, it is still one of the most common cancers of the reproductive system seen in women in the developing countries.
The Cervix
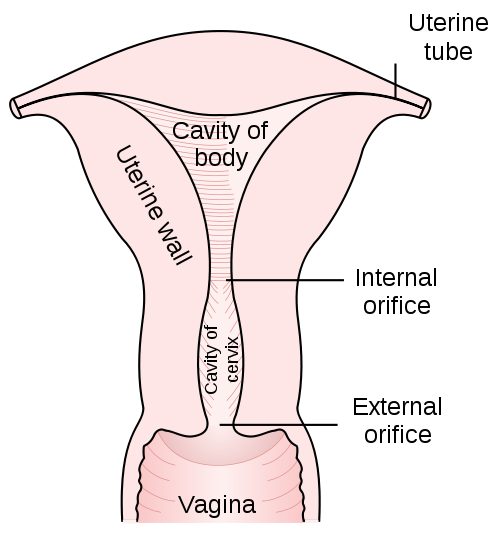
The uterus is a pear-shaped organ, consisting of the body above and the narrow lower part known as the cervix. The cervix is about 2 to 4 cm long and is divided from the body of the uterus by a slight constriction on the outside known as the isthmus, and by the internal os on the inside. The upper part of the cervix, towards the uterus, is known as the endocervix. The portion of the cervix that enters into the vagina (exocervix) divides the vagina into the anterior fornix in front, posterior fornix behind and the two lateral fornices on either side. The circular or oval opening of the cervix into the vagina is known as the external os.
Picture from Wikimedia Commons
Location of Cervical Cancers
The wall of the cervix consists mainly of fibrous tissue, with some amount of muscle fibers and elastic tissue. The endocervix is lined by columnar cells, while the exocervix is lined by squamous cells. The area where the two cell types meet is where most cervical cancers originate. This is known as the squamocolumnar junction or the transformation zone. Squamous cell carcinomas are most common cervical cancers accounting for some 80% to 90% of cervical cancers, followed by adenocarcinomas.
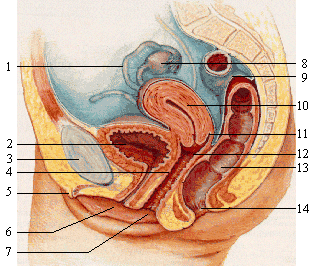
(1) fallopian tube; (2) bladder; (3) pubic bone; (4) Grafenberg spot; (5) clitoris; (6) urethra; (7) vagina; (8) ovary; (9) sigmoid colon; (10) uterus; (11) fornix; (12) cervix; (13) rectum; (14) anus
Picture from Wikimedia Commons
Cervical cancer may spread locally into the deeper layers, or into the adjacent tissues of the uterus and vagina, or to the bladder, rectum, and the pelvic wall. It may metastasize to distant sites such as the lungs, liver, bone and lymph nodes through the blood stream or lymph vessels. Lymphatic invasion may occur initially to the paracervical lymph nodes, then into the hypogastric and external iliac lymph nodes, and subsequently into the common iliac and para-aortic lymph nodes.
Pre-Cancerous Cervical Lesions
The transition phase, where the normal, healthy cells are showing some abnormalities is the pre-cancerous stage. It is also known as carcinoma in situ, cervical intraepithelial neoplasia (CIN), dysplasia, or squamous intraepithelial lesion (SIL). Most cervical cancers develop slowly from pre-cancerous growths into invasive carcinoma. Not all pre-cancerous lesions, however, develop into cancers, and many of these lesions may resolve on its own without any treatment. It is crucial to detect abnormalities at the earliest possible stage like in the pre-cancerous stage.
Growth Patterns for Cervical Cancer
Different growth patterns may be seen for invasive cervical cancer, such as :
- Exophytic growth. This develops from the exocervix and is the most common variety of cervical cancer to be seen. These may look like large, cauliflower growths, which bleed easily on touch (friable). It usually involves only the superficial layer of the cervix.
- Nodular growth. This usually arises from the endocervix and grows into the deeper layers to form a firm, nodular mass.
- Infiltrative growth. This may develop either in the endocervix or exocervix to form a stony-hard cervix without any visible ulcerative or exophytic growth.
- Ulcerative growth. The destruction and death of tissue mass over the growing tumor gives rise to an ulcerative growth. There may be associated infection, resulting in the discharge of pus.