Dehydration in Diarrhea – Symptoms, Treatment in Infants and Adults
Dehydration is low levels of water and electrolytes (salts) in the body. It arises when the loss of water exceeds the intake of water. It can happen through several routes. Fluid and salts may be lost with excessive sweating, vomiting and diarrhea.
Intestinal Water Absorption and Diarrhea
A healthy adult gets about 9 litres of water (from digestive juices and dietary intake) into the bowel daily, but excretes only 100-200 ml of it with the stool, since most of it is re-absorbed from the bowel into the blood; amount of water that body does not need is then excreted in the urine. A healthy adult can drink up to 20 litres of fluids in one day without having diarrhea.
In diarrhea, water is lost by one or more of the following mechanisms:
- In motility diarrhea, water does not have time to be absorbed because of increased bowel motility, for example in hyperthyroidism.
- In secretory diarrhea, water is actively secreted from a damaged intestinal wall, for example, in cholera
- In osmotic (osmosis = diffusion of water through a semi-permeable membrane, like intestinal mucosa), certain nutrients that can not be absorbed, like fructose in fructose malabsorption, drag water into intestine.
- In exudative (Latin exudate = ooze) diarrhea, water and proteins ooze from inflamed ulcerated intestinal mucosa, for example, in ulcerative colitis.
Over 20 litres of water (and electrolytes) may be lost in severe diarrhea in one day.
Symptoms of MILD Dehydration
Mild dehydration may develop in a couple of hours. Symptoms include:
- Dry mouth (in infants: only few tears when crying)
- Thirst – NOT a reliable symptom of dehydration; it may be absent, especially in children and old people
- Reduced amount (less than usual) of morning urine (in infants: no wet diaper for 3 hours)
- Fatigue, dizziness
Symptoms and Signs of SEVERE Dehydration
Severe dehydration may develop within a day in a heavy diarrhea. Symptoms and signs include:
- Small amount of dark colored urine (in adults: <50 ml of morning urine; in infants: no wet diapers in 6 hours)
- Thirst (not always!)
- Rapid heartbeat
- Low arterial blood pressure
- Reduced skin turgor (tension) (1). Normally, the skin on the back of the hand flattens immediately after being pinched and released; in severe dehydration, skin loses its fullness, so fold persists for more than 2 seconds (Picture 1). In infants, the test should be performed on the abdominal skin. The test is not useful in old people with loose skin.

Picture 1. Reduced skin turgor in severe dehydration
- Muscle cramps (due to loss of sodium, potassium or magnesium)
- Extreme tiredness
- Sunken eyes or front fontanel in infants (Picture 2)
- Confusion, coma
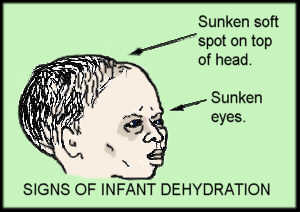
Picture 2. Signs of severe dehydration in infant
Laboratory Findings in Severe Dehydration
Blood test may show:
- Increased blood urea nitrogen (BUN), creatinine and urine specific gravity
- Levels of sodium, potassium and magnesium may be increased, decreased or unchanged (2).
Treatment of Dehydration in Adults and Children after Age of 2
Treatment of mild dehydration is by drinking water, tea, orange, lemon, grapefruit or banana juice, re-hydration solutions (e.g. Pedialyte, Infalyte, Naturalyte, Rehydralyte, etc.) or sport drinks (e.g. Gatorade), available in food stores without prescription.
Drinks to avoidin dehydration: caffeinated and alcohol drinks, diet soda sweetened by HFCS or sorbitol, milk and high-fructose fruit juices (like apple, pear, prune or peach juice) that may all aggravate diarrhea.
Treatment of severe dehydration is by intravenous fluids (in hospital), which can replace lost water and electrolytes (sodium or potassium) quickly.
Treatment of Dehydration in Small Children
Children under two years of age are more susceptible to dehydration because of their low weight. Infants with any extent of dehydration should be checked by a doctor who can prescribe appropriate oral rehydration solution (ORS). Breastfeeding should continue and ORS given. Plain water is not enough since it doesn’t contain electrolytes (Na, K) lost in diarrhea.
If a doctor can not be contacted and ORS is not available, a homemade rehydration solution may be prepared (exact amounts should be used!) (2):
- 1 liter of safe drinking water (boiled and cooled down to room temperature),
- 1 level teaspoon (5g) salt (NaCl),
- 8 level teaspoons (40g) sugar (sucrose),
- (100 ml of orange or banana juice, if available, as source of potassium, and to improve the taste).
Fluid should be given by a teaspoon until the amount of urine returns to normal and becomes clear. If baby vomits, rehydration should be tried after 10-15 minutes again. If baby is on formula, switching to a lactose-free formula should be tried. Cow’s milk and undiluted fruit juices should be avoided. In poor countries, WHO-ORS (oral rehydration solutions provided by World Health Organization) powdered packages are available. Water should be boiled before preparing the solution; a fresh solution has to be prepared every day.
NOTE: If oral rehydration is not possible from any reason, a doctor should be visited promptly.
Complications of Dehydration
Complications of dehydration include seizures, shock with rapid heart beat and shallow breathing, kidney failure (no urination), brain edema, coma and finally death. Permanent damage of the brain and kidneys may occur.
About 2.2 million young children worldwide (about 50 children in US) die every year from dehydration caused by diarrhea.
Related Articles:
References:
- Skin turgor (nlm.nih.gov/medlineplus)
- Laboratory tests results in dehydration (labtestsonline.org)




