Kidney Dialysis Methods, Machine and Indications for its Use
One of the most important functions of the kidneys in a healthy individual is to filter and remove harmful waste products from the blood. Furthermore, by regulating the amount of urine excreted, the kidneys can help to maintain the fluid balance of the body. Blood electrolytes such as sodium, potassium, and bicarbonate levels are maintained by healthy kidneys, which are also important in controlling blood pressure. However, in circumstances where the kidneys are unable to perform these functions due a person developing end-stage kidney failure, there are usually two options available – kidney transplant or renal dialysis, which come under the term renal replacement therapy.
What is Dialysis?
Renal dialysis or kidney dialysis is a process that takes over the functions of the failed kidneys by removing harmful waste substances from the blood. Short-term dialysis may be conducted in some cases of acute kidney failure, where there are chances of improvement of kidney function following treatment. Long-term dialysis is necessary in patients where there is irreversible damage to the kidney and is therefore the only means of sustaining life without a kidney transplant. Despite the life-saving function of dialysis, it is not able to replace the activity of health kidneys. The overall health of a person on dialysis is therefore significantly impaired and only a kidney transplant is able to resolve this.
Dialysis may be done in any of the following places :
- An independent dialysis unit or clinic that is not part of a hospital,
- At a hospital, or
- In a patient’s home.
A special diet needs to be followed by patients on dialysis. Dietary changes include limiting the amount of fluid intake and consuming a diet that is low in sodium, potassium, and phosphorus. Protein intake should be adequate but not in excess.
Methods of Dialysis
Renal dialysis is usually done by either of the two methods – hemodialysis or peritoneal dialysis. The method used for a patient in need of dialysis is determined by various factors. The benefits and risks will also have to be considered.
Hemodialysis
In this procedure, the toxic waste products, extra salt, and water are filtered and removed by means of a machine using a special type of filter, known as a dialyzer.
Peritoneal dialysis
This procedure makes use of the peritoneal membrane (the inner lining of the abdomen) to filter and get rid of the harmful waste products, excess salt, and water.
The Dialysis Machine
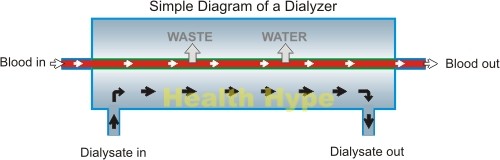
The dialysis machine filters a patient’s blood and removes waste products and excess fluid. Through the AV fistula, blood is passed on to the dialysis machine through plastic tubing. It is then carried to the dialyzer, which is a large canister containing thousands of small fibers that form a semi-permeable membrane which filters out impurities. Fresh dialysis solution (dialyzing fluid) is pumped around the filters while the blood runs through it, separated by the thin membrane.
Waste products and excess fluid from the blood pass through the fibers in the membrane into the dialysis solution by the process of diffusion. The dialysis solution (dialysate) or cleansing fluid helps to carry away the waste products and excess fluid. The used dialysate is then discarded. The newly filtered blood is passed through a bubble trap which ensures that there are no air bubbles in the blood. The blood is then returned to the body by the way of a vein.
How does the dialyzer work?
The mechanism behind dialysis may seem complicated but is rather simple. It is based on the effect of diffusion. The dialyzing fluid has less solutes (dissolved substances) than the blood. Therefore fluid, waste and electrolytes will flow out of the blood and into the dialyzing fluid (diffusion) due to the concentration gradient. The blood and dialyzing fluid are constantly flowing to optimize the diffusion from the blood to the fluid and increasing the flow of the blood, dialyzing fluid or both can optimize the diffusion even further.
What is the composition of dialyzing fluid?
Dialyzing fluid has many of the same electrolytes and non-electolytes as blood. Most of these substances are in much lower concentration than normal blood or the blood of a patient with a kidney disorder (uremic blood). This, however, is not the case for electrolytes and non-electrolytes such as magnesium, bicarbonate, lactate and glucose which may be at the same levels as uremic blood or even higher since the intention is not to remove it. Conversely, there is no phosphate, urea, urate, sulfate, or creatinine in the dialyzing fluid as this is high in the uremic blood and the intention is to remove as much of these substances as possible during dialysis.
How much blood is in the dialysis machine and flowing through the dialyzer?
There is usually less than 500 milliliters (less than a pint) of blood in the dialysis machine at any one time. The rate of blood flow through the machine may be several hundred milliliters at per minute. The blood flow back into the vein of the patient is either continuous or intermittent. Blood does not coagulate (clot) in the machine because a small amount of heparin (anti-clotting agent) is added to it which also helps the flow of the blood.
How efficient is the dialysis machine?
Modern dialysis machines are very efficient and can remove about 100ml to 200ml of urea from the blood in a minute. This is actually more efficient than the healthy kidney which is only able to filter out about 70ml of urea per minute. However, the healthy human kidney is constantly active while dialysis in only undertaken for a few hours 2 to 3 times a week. Furthermore the regulation of water, electrolyte and non-electrolyte levels with a dialysis machine is not able to match the kidney’s ability as this is in a constant state of flux to maintain the optimum levels and therefore homeostasis.
Indications of Dialysis
Who will need dialysis?
Dialysis becomes necessary when, due to extremely poor kidney function, waste products build up sufficiently in the body to cause illness that becomes life-threatening. This advanced and permanent kidney failure is known as end-stage renal disease (ESRD). Renal replacement therapy is required to sustain the patient’s life. While a kidney transplant may be preferred in some cases, it may not always be possible, and dialysis becomes the alternate option. A kidney transplant may be done at a later date if possible, otherwise lifelong dialysis may become necessary.
The main indicators of progressive kidney failure are serum creatinine and blood urea nitrogen (BUN). Dialysis may be indicated when the creatinine clearance (the comparison between the blood and urine creatinine level) falls to 10-12 cc/minute.
In some cases, dialysis may be necessary even though the creatinine clearance is well above to 10-12cc/minute but there is excess accumulation of water in the body with ankle swelling, breathing difficulty, extremely high blood pressure, nausea, vomiting, and poor mental concentration.
Dialysis usually becomes necessary when there is only about 10 to 15 % of normal kidney function left. It should begin before kidney function has deteriorated to such a state that life-threatening complications are evident. Chronic renal failure may be caused by long-term diabetes mellitus (sugar diabetes), hypertension (high blood pressure), glomerulonephritis, and polycystic kidney disease.
Dialysis on a temporary basis may be done in some cases of acute kidney failure, where the kidneys are expected to regain their function after adequate treatment of the causative factor, such as a heart attack.