Temporal Arteritis (Giant Cell Arteritis) Causes, Symptoms, Treatment
Arteries are blood vessels that carry oxygen-rich blood throughout the body. The exception is the pulmonary artery emanating from the right side of the heart which carries oxygen-deficient blood to the lungs for re-oxygenation. Arteries have thicker walls than blood vessels which is muscular and elastic. The muscles allows the arteries to constrict or dilate in order to regulate blood flow to an area and the elasticity allows for recoil to allow blood to be propelled throughout the body at suitable pressure. Sometimes the wall of the arteries can become inflamed and this condition is known as vasculitis. There are different types of vasculitides (plural of vasculitis) and the most common of these is a condition known as temporal arteritis. It is also known by other names like giant cell arteritis (GCA) and cranial arteritis.
What is temporal arteritis?
Temporal arteritis is an inflammatory condition that mainly affects the temporal arteries. The common symptoms of temporal arteritis is a headache on the sides of the head (temples) where the temporal arteries are located. The other popular name of temporal arteritis is giant cell arteritis because large cells form in the swollen walls of the arteries. Temporal arteritis is commonly discussed in conjunction with a condition known as polymyalgia rheumatica (PMR). Almost 50% of people with temporal arteritis have PMR, but only about 10% to 20% of people with PMR have temporal arteritis. The exact reason why temporal arteritis occurs is unclear but it is mainly seen in the elderly, usually starting after 50 years of age and is more common in the 70 year age group.
Meaning of temporal arteritis
The term temporal arteritis can be misleading because the temporal arteries are not the only vessels that are affected in this disease. Temporal arteritis is a systemic condition marked by inflammation of the arteries. This means that any artery in the body can be affected although it occurs mainly in the large to medium-sized arteries. Since the temporal arteries are the most commonly affected, whether in conjunction with other arteries or on its own, it is therefore referred to as temporal arteritis. However, the other common name, giant cell arteritis, may actually be a more accurate term to describe the disease.
The exact cause of temporal arteritis is unknown. However, the disease mechanism is fairly well understood. Certain chemicals from a type of immune cell, in this case a T-lymphocyte, causes inflammation of the artery wall. These chemicals known as cytokines have a specific function in the body’s defense response against invading microorganisms. However, in conditions like temporal arteritis it affects the body’s tissues even in the absence of any threat. Over time the repeated inflammation of the artery wall causes its tissues to increase in size and some very large cells form within it which are called giant cells. This thickening of the artery wall causes narrowing of the lumen thereby impeding the normal blood flow.
Temporal arteritis symptoms
The signs and symptoms of temporal arteritis are often mistaken for other conditions and therefore the condition is often missed in the early stages. The main symptoms of temporal arteritis are a headache and tenderness over the sides of the head. Some of the other symptoms may be due to polymyalgia rheumatica (PMR) which often co-exists with temporal arteritis.
Headache
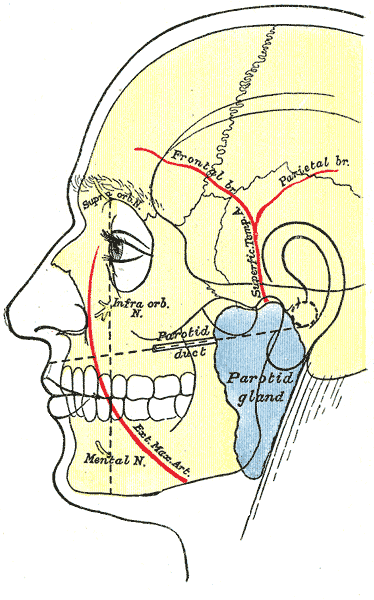
The headache in temporal arteritis is localized to the temples, which are the sides of the head where the temporal arteries are located – one on either side. The pain is usually severe and often affects both sides simultaneously (bilateral). However, in some cases the pain of the headache may only be on one side of the head or even cause a frontal headache where the pain is more towards the forehead. The pain may also extend to the eyes.
Tenderness
The sides of the head where the temporal arteries are located are usually tender in temporal arteritis, even if there is no headache. This means that pressure over the area causes discomfort or pain. The tenderness may extend to the scalp and daily activities like brushing the hair can cause pain.
Jaw Pain
There is often jaw pain in temporal arteritis and this can be more prominent when chewing. In some cases the pain may extend all the way down from the temples, across the jaw and even extend as far as the shoulders when polymyalgia rheumatica is present.
Vision Problems
There are various different types of vision problems in temporal arteritis which is more likely to be present in severe cases where there is significant narrowing of the temporal arteries. These vision problems may affect one eye only or both eyes simultaneously. A person may report a blurred vision, double vision or even partial or complete loss of vision (blindness). Although these symptoms develop over time and may come and go, it is possible for there to be a sudden loss of vision in one eye. Loss of vision in temporal arteritis may be permanent.
Other Symptoms
Temporal arteritis may also present with fever, loss of weight, night sweats, fatigue and depression. These non-specific symptoms are also present in polymyalgia rheumatica and can often be misleading as it is also seen in other, more common conditions and in particular systemic infections.
Temporal Arteritis Causes
The exact cause of temporal arteritis is unknown. The abnormal immune response in temporal arteritis causes sections of the artery, and most commonly the temporal arteries, to become inflamed. This leads to swelling and over time there is also thickening of the arterial wall. These changes in the arterial wall does not happen over the entire artery but in sections. This means that inflamed sections of the arterial wall may be interspersed among sections of a normal wall. Although the cause of temporal arteritis has not as yet been identified, there are certain risk factors which could be indicative of a yet unknown etiology. These risk factors includes age, gender, infections, certain medication, polymyalgia rheumatica or genetic factors.
Risk Factors for Temporal Arteritis
The risk factors below means that temporal arteritis is more likely in certain people. It does not mean that every person who has one or more of these will develop temporal arteritis.
Age
Temporal arteritis is more likely to occur after the age of 50. The average age when temporal arteritis appears to commence is about 70 years old. This indicates the stronger risk of temporal arteritis in seniors.
Gender
Temporal arteritis is more frequently seen in females and women may be as twice as likely than men to develop temporal arteritis.
Infections
Temporal arteritis may be related to some infectious condition but is not due to an infection. This means that a previous infection and the immune response to it may increase the likelihood of developing temporal arteritis at a later stage even though the infection has resolved. It is as yet unclear whether this may also be related to the use of certain medication in the course of the treatment of this infection.
Polymaylgia rheumatica
Polymyalgia rheumatica (PMR) has a close association with temporal arteritis. This condition is marked by intense inflammation of the tissues surrounding joints. There is muscle pain at around several joints like in the neck, shoulders, lower back, hips and thighs. The cause of polymyalgia rheumatica is not well understood but appears to be similar to temporal arteritis. It is also unclear whether the mechanism of polymyalgia rheumatica may actually cause temporal arteritis in some cases.
Family history
Both temporal arteritis and polymyalgia rheumatica are more likely to occur in individuals with a family history of these conditions indicating a possible genetic component.
Temporal Arteritis Diagnosis
The diagnosis depends on the medical history, findings of the physical examination and subsequent investigations. The main blood tests that are conducted for temporal arteritis are to check the erythrocyte sedimentation rate (ESR) and the levels of C-reactive protein (CRP). Other investigations may include imaging studies such as magnetic resonance imaging (MRI), duplex ultrasound and positron emission tomography (PET). The preferred method of diagnosing temporal arteritis is with a temporal artery biopsy. Here a small portion of the temporal artery is removed and examined under a microscope. It can sometimes be misleading since not all sections of the temporal artery is affected.
Biopsy Video
The video below is of a temporal artery biopsy. The content is graphic and sensitive viewers are advised to be cautious. Sourced from Google Videos.
Treatment of Temporal Arteritis
Treatment for temporal arteritis needs to be commenced immediately once the condition is suspected even before a diagnosis can be confirmed. This is to avoid any complications of temporal arteritis like permanent blindness, a heart attack, stroke, deafness, nerve damage or aortic aneurysm. The main treatment involves the use of corticosteroids like prednisone or methylprednisolone. Corticosteroids are very effective anti-inflammatory agents but long term use of high doses is associated with a host of side effects. Other drugs like methotrexate may also be used to suppress the immune system and reduce inflammation. Since there is a risk of blood clots forming in the narrowed vessels in temporal arteritis, drugs like aspirin are prescribed to reduce the formation of clots which may lead to strokes or blindness.
References
1. Giant cell arteritis. Emedicine Medscape
2. Temporal arteritis. Patient.co.uk