Sacrum and Coccyx (Tailbone) of the Spine Anatomy and Pictures
Sacrum
Anatomy
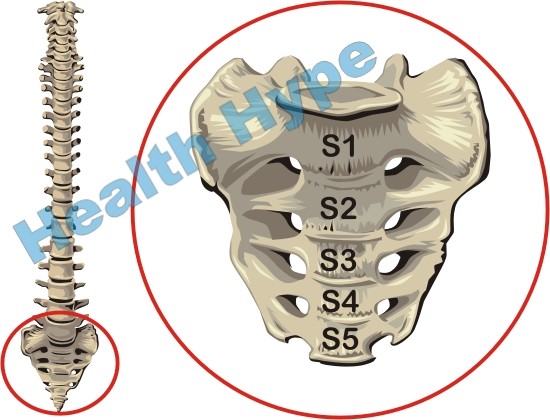
The sacrum is a single wedge-shaped bone formed by the fusion of five sacral vertebrae. In childhood, the sacral vertebrae are separated by intervertebral discs in much the same manner as the upper parts of the spinal column. However, around the age of 20 these vertebrae start to fuse by ossification of the discs. This is a gradual process and it is not uncommon for ossification to only be completed up to or even beyond 40 years. The sacrum is wider in proportion to the length in females although the first sacral vertebra (S1) is larger in males.
The vertebral column which houses the spinal cord continues in the sacrum. The sacral canal contains a bundle of spinal nerve roots known as the cauda equina (Latin for ‘horse tail’). These nerves exit the sacrum through the four pairs of sacral foramina on the anterior (pelvic) and posterior (dorsal) surfaces.
The pelvic surface faces anteriorly (front) and is smooth and concave. Examination of the pelvic surface reveals four transverse lines which indicate where the sacral vertebrae have fused. The dorsal surface faces posteriorly and is rough and convex. The longitudinal ridges in the middle of the dorsal surface is known as the median sacral crest and is the remnants of the spinous processes of the sacral vertebrae. The transverse processes of the sacral vertebrae form the lateral sacral crests.
Weight-Bearing Function
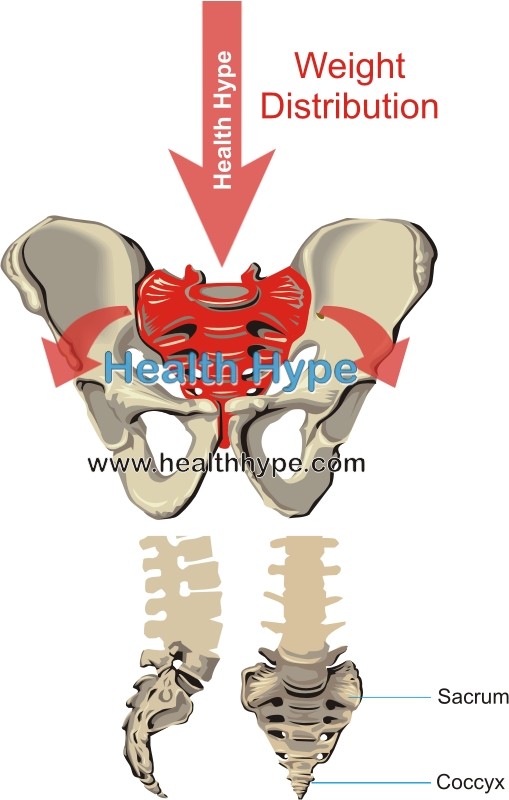
The sacrum is lodged between the hip bones where it provides strength ad stability to the pelvis for the attachment and movement of the limbs and also to transmit the body weight of the upper half of the body to the pelvic girdle. The upper half of the sacrum is wider and larger because of its weight-bearing functions. The lower half does not play a role in these activities when standing and is therefore not as bulky.
The first of the sacral vertebrae, S1, is in direct contact with the largest movable vertebra in the body – L5. The weight of the entire upper body is carried by L5 which then transmits this weight to the sacrum. The upper half of the sacrum in turn transmits this weight to the pelvic girdle.
The sacrum has four important sites where it articulates with surrounding bones.
- The base of the sacrum is formed by the superior surface of the S1 vertebra which articulates with L5. This is known as the lumbosacral joint. The angle formed by the L5 vertebra and sacrum is known as the lumbosacral angle which is between 130 to 160 degrees.
- The apex of the sacrum has an oval facet which allows the sacrum to articulate with the coccyx (tailbone).
- The lateral aspects of the sacrum has auricular surfaces which allow it to articulate with the ilium (the largest bone of the pelvis. This is known as the sacro-iliac joint.
Coccyx
Anatomy
The human tailbone is a remnant of the of the embryonic tail-like protrusion of the skeleton (caudal eminence). It is normally present in the embryo towards the end of he 4th week till around the 8th week. The coccyx is formed by the fusion of four coccygeal vertebrae which forms a small triangular bone at the base of the spinal column. These vertebrae are fairly underdeveloped when compared to those of the cervical, thoracic and lumbar regions of the vertebral column. The first coccygeal vertebra (Co1) usually fuses with the sacrum with age while the lat 3 coccygeal vertebrae fuse together to form the coccyx as a single bone.
Weight-Bearing Function
Unlike the other vertebrae, the coccyx does not play a role in supporting the body weight when standing. Its anterior flexion when sitting however, indicates that it may bear some weight during sitting. It is nevertheless an important part of the spinal column as it serves as a site of attachment for various muscles and ligaments.
Palpation
The coccyx has an inner facing pelvic surface and outer posterior surface. The coccyx can be palpated in the intergluteal cleft (the space between the two ‘cheeks’ of the buttock). Its top lies about 2.5 cm to the back and above the anus and is examined by a medical professional through the insertion of gloved finger into the anal canal.