Autoimmune Gastritis (Stomach) Causes, Signs and Symptoms
Gastritis is the term for inflammation of the stomach. As a hollow sac, it is the walls of the stomach that are inflamed to varying degrees. This may sometimes be isolated to the superficial inner lining of the stomach (mucosa) or it can extend through the entire wall of the stomach. Persistent inflammation leads to ulcers, which can be deep or shallow. Most cases of chronic gastritis are due to H.pylori (Helicobacter pylori) infection or the excessive and/or long term use of NSAIDs (non-steroidal anti-inflammatory drugs). However, a minority of chronic gastritis cases are not due external factors but arises with an immune-mediated reaction and is known as autoimmune gastritis. It needs to be considered as a possible cause of chronic gastritis that is not associated with H.pylori infection or NSAID use.
What is autoimmune gastritis?
Autoimmune gastritis is a type of chronic stomach inflammation due to the action of the immune system against stomach tissue and its components. It causes destruction of the stomach tissue with progressive atrophy of the stomach and is therefore also referred to as autoimmune atrophic gastritis or autoimmune metaplastic atrophic gastritis. Autoimmune gastritis leads to low gastric acid secretion (achlorhydria) and pernicious anemia (megaloblastic anemia) due to vitamin B12 deficiency and it is a known risk factor for gastric cancer.
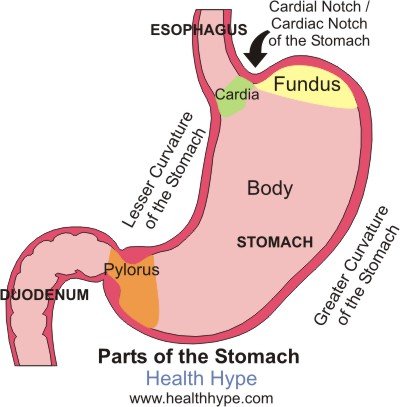
The stomach is the first major organ of digestion lying between the esophagus and duodenum of the small intestine. There are three types of cells in the gastric wall – mucus, peptic and parietal cells. With regards to autoimmune gastritis, it is the parietal cells that are targeted by the immune system. These cells produce hydrochloric acid (HCl) and intrinsic factor (IF).
HCl is an important component of chemical digestion while intrinsic factor is needed for the absorption of vitamin B12. When the parietal cells are destroyed, the level of the substances it secretes are affected and this ultimately disrupts its respective roles in digestion and absorption. However, the other cells like peptic cells are also destroyed in the process although the immune system is not specifically directed at these cells in the way it is towards the parietal cells.
Pathophysiology of Autoimmune Gastritis
Antibodies are formed against the parietal cells, hydrogen-potassium ATPase (H+,K+-ATPase of the proton pump) and and intrinsic factor (autoantigens). These autoantibodies direct the immune response against this otherwise normal tissue and its components. This reaction appears to be mediated specifically by the CD4+ T-cells. Most of the damage of the parietal cells arises in the body and fundus of the stomach while the antrum of the pylorus and cardia is spared entirely or at least to a very large degree.
Typically the inflammation and subsequent destruction and atrophy of the tissue is extensive. It usually affects the entire area but sometimes can be patchy with the isolated normal mucosa appearing like small nodules or polyps (pseudopolyps). As acid production drops with parietal cell destruction, the body tries to compensate by increasing the production and secretion of gastrin (digestive hormone). Usually gastrin stimulates gastric acid production by directly acting on the parietal cells and indirectly by acting on the enterochromaffin-like (ECL) cells. Hypergastrinemia (elevated blood levels of gastrin) continues to stimulate the ECL cells in autoimmune gastritis thereby causing it to increase in number (hyperplasia). The areas where atrophy occurs (fundus and body) may display abnormal cellular changes (metaplasia).
Causes of Autoimmune Gastritis
Autoimmune gastritis is mainly an inherited disorder. It is associated with many other hereditary conditions including Hashimoto thyroiditis, type I diabetes mellitus, Addison disease, primary hypoparathyroidism, Graves disease, myasthenia gravis, and Lambert-Eaton syndrome. However, the exact genes for autoimmune gastritis has yet to be identified. There also appears to be an association with chronic H.pylori infection but the exact link and mechanism is unclear. Other factors that need to be considered include long term use of proton pump inhibitors (PPIs) and gastrectomy (surgical removal of part of the stomach).
Signs and Symptoms of Autoimmune Gastritis
The clinical features are largely due to the pernicious anemia. While low gastric acid levels may affect digestion of several nutrients, it is usually minor if small portions of the gastric wall is affected. Instead the vitamin B12 deficiency is more prominent. The condition usually develops gradually and takes decades to reach a point where the deficiency causes significant clinical effects. The signs and symptoms in this regard may therefore include :
- Abnormal sensations particularly in the legs (paresthesia) and numbness.
- Smooth red tongue (glossitis).
- Diarrhea.
- Mouth pain (stomatodynia).
- Cracking at the corner of the lips.
- Weakness of the limbs.
- Mild personality changes.
- Poor memory.
- Sometimes depression.
- Malaise.