Calciphylaxis (Calcified Skin Blood Vessels)
What is calciphylaxis?
Calciphylaxis is a condition where there is abnormal deposition of calcium in the body primarily affecting certain small blood vessels and leading to skin damage. It is also referred to as vascular calcification as the blood vessel becomes hardened due to the calcium deposition. The main blood vessels affected in calciphylaxis are the tiny arterioles supplying blood to the subcutaneous fat and the skin above it. It can be life threatening and most deaths arise from complications rather than from calciphylaxis itself. Although the skin is primarily affected in calciphylaxis, the same process can occur in the tiny arterioles of internal organs. The consequences of internal organ involvement can be life-threatening even without an infection.
How common is calciphylaxis?
Overall calciphylaxis is a rare. It is mainly seen in people with end stage renal disease (ESRD) where the body is unable to maintain the normal levels of different minerals like calcium. Although calciphylaxis is uncommon in the general population with normal kidney functioning, the condition may be linked in these groups to the aluminum toxicity, vitamin D supplementation and iron dextran injections. Calciphylaxis has a high mortality rate leading to death in as many as 80% of patients with the condition.
Calciphylaxis Process
Calcification of blood vessels
Blood vessels are flexible with a smooth inner lining. This allows blood to flow through it freely. Fluid from the blood containing nutrients and oxygen pass out of the vessel and into the tissue. Fluid around the cells containing wastes and carbon dioxide enter the blood vessel to be carried away and eliminated. Calcification of the blood vessels affects these processes in several ways. The deposition of calcium can make the blood vessels rigid, hampers smooth blood flow and leads to blood clot formation.
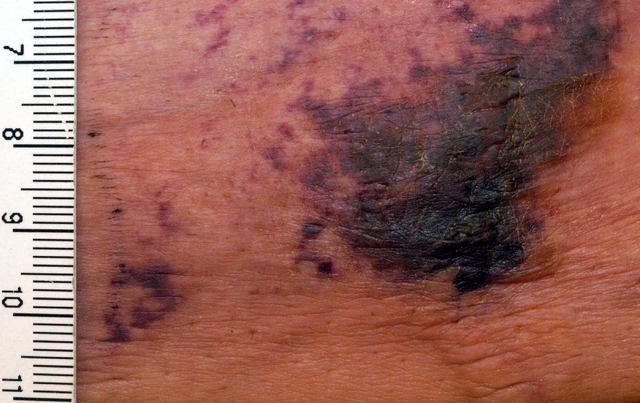
Tissue death and gangrene
Reduced blood supply to the area leads to tissue damage and death as the fat and skin is deprived of nutrients and oxygen. It is the formation of blood clots within the vessel that blocks blood flow. Areas of the skin become painful and tissue death occurs (necrosis). Stasis of blood and cell death leads to a purple-blue to black color of the affected skin. Gangrene sets in, ulcers may form on the skin and it can become infected with bacteria. The infection can spread and lead to life-threatening complications like septicemia.
Signs and Symptoms
Calciphylaxis causes pronounced skin symptoms starting from discoloration of the skin and leading to gangrene with ulcers. The typical lesions seen with calciphylaxis on the lower abdomen, buttocks, thighs, lower legs and feet. There is itching, a burning sensation and pain at the affected site.
Early lesions
- Purple mottling of the skin
- Bleeding under the skin with blood-filled blisters
Intermediate lesions
- Star-shaped purple lesions which are black in the center
- Lesions are firm and very tender
Late lesions
- Dry gangrene
- Multiple deep ulcers
Picture from Wikimedia Commons
Causes of Calciphylaxis
Calciphylaxis is a result of calcium-deposition in the walls of the blood vessels. In almost all cases this is due to abnormal calcium levels in the blood and kidney disorders. However, in a small number of cases the blood calcium levels are normal and there is no kidney dysfunction. Although the parathyroid gland plays a central role in calcium metabolism within the body, even in the absence of parathyroid abnormalities calciphylaxis can occur.
Kidney failure
The kidneys regulate the levels of various minerals, electrolytes and other substances in the bloodstream. With chronic kidney failure and end-stage renal disease (ESRD), the kidney’s ability to regulate calcium levels are drastically impaired. Calcium levels in the blood become elevated and there is an increased chance of calcium deposition. Various other factors may also play a role in blood vessel calcification but kidney dysfunction is by far the main causative factor of calciphylaxis.
Other Causes and Risk Factors
- Abnormal levels of calcium and phosphorus in the blood
- Aluminum toxicity
- Blood clotting disorders and anticoagulants
- Iron dextran injections
- Hyperparathyroidism
- Medications that affect the calcium levels
- Systemic inflammatory conditions and corticosteroids that are used to treat these disorders
- Vitamin D supplementation
Tests and Diagnosis
The lesions seen in calciphylaxis are not significantly different from other vascular conditions. In particular, peripheral arterial disease (PAD) where the arteries of the legs narrow (atherosclerosis) may also present with similar skin lesions. However, the leg pulses are usually normal in calciphylaxis unlike with peripheral arterial disease. Diagnostic investigation for calciphylaxis includes :
- Various blood tests for levels of calcium, phosphorus, urea and creatinine and parathyroid hormone (PTH). Other blood tests may be conducted to identify specific causes.
- Plain x-ray
- Bone scintigraphy
- Skin biopsy
Calciphylaxis Treatment
The approach to treating calciphylaxis depends on the extent of the condition. In the event of gangrene and ulcers, wound care is of the utmost priority as an infection can progress to the point of septicemia and lead to death. Antibiotic treatment is necessary and dead tissue may be surgically removed (debridement). Restoring blood flow and oxygen supply to affected areas where tissue death has not as yet occurred is also a priority. The affected tissue can be saved through hyperbaric oxygen therapy, and “clot busting” drugs that will dissolve clots and restore blood flow.
There is no definitive treatment for calciphlaxis itself. The focus of treatment is to reduce the calcium and phosphate levels. Dietary modification may be one way of achieving these goals but medication and other therapeutic measures are usually needed. These measures may include :
- Calcimimetics are drugs that mimic insulin thereby “tricking” the parathyroid glands into reducing parathyroid hormone (PTH) secretion.
- Bisphosphonates prevent bone breakdown and therefore calcium release from the bones.
- Dialysis to help normalize the mineral, electrolyte and waste levels in the blood.
- Parathyroid gland removal (parathyroidectomy) is hyperthyroidism is the cause of calciphylaxis.
Complications of Calciphylaxis
- Amputation of a gangrenous limb in the event of extensive gangrene and poor wound management.
- Septicemia with poor management and delayed treatment particularly if there are is non-healing ulcers.
- Abnormally low blood calcium levels (hypocalcemia) with the use of calcium-lowering drugs and surgical removal of the parathyroid gland.
- Heart attack (myocardial infarction), gastrointestinal bleeding and organ death if internal organs are also affected with calciphylaxis.
References :
http://dermnetnz.org/systemic/calciphylaxis.html
http://www.mayoclinic.org/calciphylaxis/
http://emedicine.medscape.com/article/1095481-overview