How To Diagnose Lupus (SLE)? Symptoms and Tests
Lupus is a broad term for a group of autoimmune conditions. A mild type is cutaneous lupus erythematosus, the most notable form being discoid lupus erythematosus (DLE), which primarily affects the skin. A greater concern for most people is systemic lupus erythematosus (SLE) which can affect several organs throughout the body. Lupus can also be caused by using certain drugs and this is known as drug-induced lupus. There are other newborn and childhood variants that are less commonly seen. The problem with diagnosing lupus is that many of the signs and symptoms resemble other more common conditions.
Most people focus on SLE when they think of lupus. The terms lupus and SLE will be used interchangeably in this article. Severe forms of SLE can be deadly but milder forms can be well controlled with drugs. However, even these milder cases can affect the quality of a person’s life. SLE is relatively uncommon. It tends to begin earlier in life, usually around the 20s and 30s but the onset may range from 15 to 50 years of age. Almost 9 out of 10 people who suffer with SLE are women. Asian and African women are at a significantly higher risk of developing SLE.
Diagnosing SLE
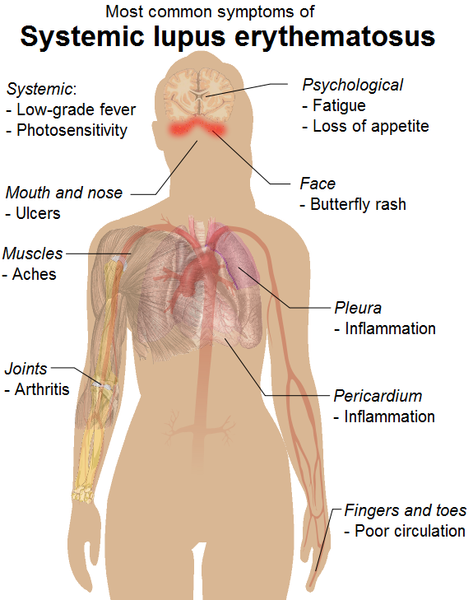
The presentation of lupus can vary greatly from one person to another. In most cases the condition is mild and symptoms may be missed in many instances. However, there are acute episodes or flareups that last for short periods during which symptoms become intense. The signs and symptoms of SLE can vary significantly over time and diagnostic investigations are necessary to confirm the condition. It is an autoimmune condition meaning that immune system attacks the body’s tissues and organs. Therefore tests may either focus on the abnormal activity of the immune system or the common complications of lupus.
The typical triad of malar rash, joint pain and fever of unknown origin in females within the reproductive years should warrant the need for further investigations to confirm or exclude a diagnosis of SLE. According to the American College of Rheumatology (ACR) 4 out of 11 criteria should be present to confirm a diagnosis of SLE. Read more on these diagnostic criteria for SLE.
Blood Tests
Non-specific tests like a complete blood count (CBC) may indicate anemia or a low white blood cell count, both of which occurs in lupus. An erythrocyte sedimentation rate (ESR) that is faster than normal may indicate an inflammatory condition like lupus. However, these positive readings are common to other diseases as well. The antinuclear antibody (ANA) test is another investigation that may point towards lupus. If positive it indicates that the immune system is abnormally active. However, many people with a positive ANA test may not have lupus. The results of these tests should be considered in conjunction with the signs and symptoms, personal and family history.
Fatigue
Fatigue is one of the first symptoms of lupus. A person feels uncharacteristically tired and has to rest more frequently and for longer than normal. Resting may not necessarily fully relieve the fatigue. Even mild physical activities that were previously not a problem results in extreme tiredness. The level of tiredness usually does not correlate with the level of activity or the person’s physical fitness. However, fatigue is a common symptoms of many different types of diseases and is not usually sufficient to diagnose lupus.
Unknown Fever
A fever is usually associated with an infection. But in lupus, it is not an infection that is responsible for the persistent or intermittent fevers. Although a person with SLE may contract infections like any other person and experience a fever, the SLE fever is independent. It is usually a low-grade fever of unknown origin and mainly seen during acute flareups. The fever, along with unexplained fatigue, SLE facial rash, joint pain and weight changes are the main signs of SLE.
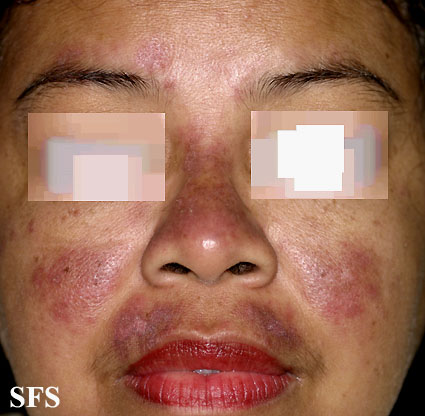
Facial Rash
One of the characteristic signs of SLE is a malar rash. It appears on the face, on both cheeks under the eyes and across the bridge of the nose. It is often described as a butterfly-shaped rash that is red to brown in color. Sometimes it can be slightly painful and itchy but often there is no sensation. Sunlight exposure may make the rash more prominent and sensitive. The SLE malar rash is sometimes confused with melasma but these two skin rashes are due to entirely different causes.
Typical butterfly-shaped SLE rash from Dermatology Atlas Brazil (courtesy Samuel Freire da Silva, M.D.)
Joint Symptoms
Joint pain (arthralgia) is another common symptom of SLE. It may be accompanied by stiffness and swelling of the joint. Often these symptoms are mistaken for joint conditions like rheumatoid arthritis (RA) especially when it occurs in younger patients and there are no other characteristic symptoms like the malar rash present. The antinuclear antibody (ANA) test may also be positive in rheumatoid arthritis and the diagnosis of SLE may be missed initially. The difference is that SLE arthritis is usually asymmetrical as compared to the symmetrical joint involvement in RA.
Weight Changes
Changes in body weight is a common constitutional symptom in SLE. Usually there is unexplained weight loss particularly when the disease is active. Patients may find difficulty gaining weight even during the remission period. However, sometimes weight gain does occur in SLE but is often associated with kidney and heart complications leading to fluid accumulation in the body. Another common cause for weight gain in SLE patients is the chronic use of corticosteroids to manage the disease. Although it is an undesirable side effect, corticosteroids should never be stopped unless a doctor advises so.
Other Features
SLE is a systemic autoimmune condition meaning that the immune system can target tissue anywhere in the body. Signs and symptoms may be seen at several sites simultaneously although it may seem unrelated. Similarly the complications that may arise may be widespread. The following features may be seen in SLE and are more likely to be noticeable in severe cases and during active periods.
- Skin – oral and genital ulcers, bluish tips of the fingers and toes (Raynaud phenomenon), hair loss.
- Musculoskeletal – muscle pain/tenderness, tendonitis and arthritis, hand deformities.
- Urinary – proteinuria, raised BUN and creatinine levels, swelling (limbs, around eyes, abdomen).
- Heart – arrhythmias, murmurs, pericarditis, myocarditis, pulmonary hypertension, heart failure.
- Respiratory – shortness of breath, pleuritis, low blood oxygen levels (hypoxia), chest pain (may also be cardiac in origin).
- Nerve and mental – confusion, poor memory, headaches, visual disturbances, sensory or motor impairment or functional loss.
- Gastrointestinal – abdominal pain/tenderness, ascites, peritonitis, pancreatitis, mesenteric vasculitis.