Inflamed Tendon (Tendonitis) – Types, Causes, Symptoms, Treatment
The muscles in the body are connected to bones by tendons. These tendons are strong. It has to constantly bear force that is generated by the contracting muscles. Like any part of the body, these tendons can be injured, strained or even cut (severed). These various tendon problems are broadly referred to as tendinopathy. It can cause pain and movement may be difficult.
What is tendonitis?
Tendonitis (tendinitis) is the term for inflammation of the tendons. Inflammation causes swelling, pain and impaired function. The swelling is not usually visible because the tendons like beneath the skin. The pain on other hand can be felt and worsens when the affected tendon has force placed on it during muscle contraction.
Most of us mistaken the tendon pain for muscle pain (myalgia). Often the muscle is also inflamed but tendonitis can occur even without muscle inflammation. There are some areas where tendonitis is more likely to occur, particularly around the large joints – shoulder, wrist, knee, lower leg and at the back of the ankle.

What happens in tendonitis?
Tendons are bands of connective tissue which attach to muscle at one end and to bone at the other. It is present with muscles throughout the body. The fibro-elastic connective tissue that make up tendons allow it to be strong yet flexible to some degree.
The point where the muscle meets the tendon is known as the musculotendinous junction (MTJ). The other end of the tendon attaches to the bone. The point where the tendon attaches to the bone is known as the osteotendinous junction (OTJ).
Muscles shorten when they contract. This pulls the tendon attached to the muscle at the musculotendinous junction (MTJ). At the other end, the tendon pulls on the bone at the osteotendinous junction (OTJ). Bones bend at the joint. This is how movement is possible.
Like any part of the body, tendons can become inflamed. Inflammation is the body’s response to injury. Heat, redness, swelling and pain are the key features of inflammation. It also affects the function of the affected tissue. Depending on the severity and duration of the tendon injury there may be micro-tears and even tendon degeneration in time. In rare cases, the tendon can rupture.
Types of Tendonitis
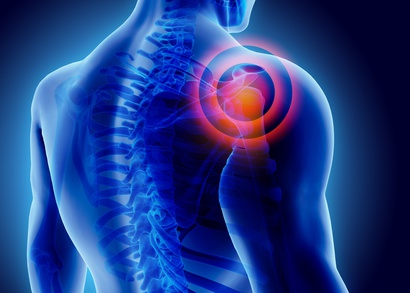
Tendonitis can occur involve any tendon anywhere on the body. However, there are certain areas that are more prone. This includes the shoulder, wrist, knee, lower leg and heel. Many of these different types of tendonitis are known by common names such as pitcher’s (thrower’s) shoulder, swimmer’s shoulder, golfer’s elbow, tennis elbow and jumper’s knee.
The tendons that are most commonly affected includes:
- Shoulder: Rotator cuff tendonitis and bicepital tendoninitis.
- Elbow: Lateral epicondylitis and medial epicondylitis.
- Knee: Patellar and popliteus tendonitis.
- Lower leg: Posterior tibial tendonitis (shin splints).
- Heel: Achille’s tendoninitis.
Causes of Tendonitis
Although trauma on an area of the body, like a blow, can injure and inflame the tendons, most of the time tendonitis is due to an overuse injury. It may occur suddenly with severe strain being placed on the tendon. However, this is not common. The most common causes of tendonitis are due to repetitive stress injuries. This is where the same movement is done repetitively which strains the tendon.
Tendonitis can affect any person of any age but it is more common with certain occupations and physical activities. Older people are also at greater risk as the tendons become less flexible with age. Jobs involving repetitive actions also increase the risk of tendonitis. There is also a greater risk of tendonitis among professional sportspeople, as is seen with sports like in most ball games, running and swimming.
However, there is a risk of tendonitis even without it being related to an occupation or sports. This is seen more often with modern technology these days. For example, prolonged use of mobile phones can cause neck and thumb problems known as text neck and texting thumb, respectively.
Signs and Symptoms
Most of the time it is difficult to differentiate between muscle strain and tendon strain because the symptoms are largely similar. The muscles and tendons may both be strained at the same time.
- Pain is one of the most common symptoms. It can be felt at the affected area and tends to worsen with movement.
- Tenderness is another symptom of tendonitis. It is typically felt at the point where the tendon attaches to the bone (osteotendinous junction).
- Swelling also occurs with tendonitis although it is not always evident for deeper lying muscles. The swelling tends to be mild.
Tendon rupture is a serious complication that can arise with severe or repetitive tendonitis. The pain in a tendon rupture is severe, arises suddenly and typically there is a snap or pop that is heard or felt when the rupture occurs. Another complication that may occur is tendinosis, which is a degeneration of the tendon that may develop with prolonged tendonitis.

Treatment of Tendonitis
In most cases tendonitis does not require any specific medical treatment. Supportive measures are sufficient. R.I.C.E. (rest, ice, compression and elevation) helps to reduce pain and prevent any further worsening of the condition. Medication may help with pain management and surgery is not usually warranted for most cases of tendonitis.
- Rest: Try not to use the affected limb excessively for at least 24 to 48 hours. There is no specific time period that is recommended but the pain, tenderness and swelling should subside before normal activity can be continued.
- Ice: Apply an ice pack or cold compress on the affected area. This should be done for the first 24 to 48 hours following the injury or onset of symptoms.
- Compression: Bandaging the area may be helpful but should not be applied too tightly. Elastic bandages are preferable.
- Elevation: Raising the affected limb can be helpful. This is usually only necessary when swelling is present and only for the lower limb.
- Medication: Over-the-counter (OTC) pain relievers can be used for pain management. Corticosteroid injections may be required for more severe cases.
- Physical therapy: Physical therapy is usually helpful, especially for severe or repetitive cases of tendonits.
- Surgery: Surgical procedures may only be considered in chronic cases where there is scar tissue formation or if there is tearing of the tendon.
References:
- Tendinitis. Mayo Clinic
- Ruptured tendon. WebMD

