Knee Osteonecrosis (Bone Death)
What is knee osteonecrosis?
Knee osteonecrosis (osteo = bone, necrosis = death) refers to the condition, in which knee pain results from death of a segment of bone. In knee osteonecrosis, the otherwise normal bone circulation in the knee region is impaired the diminished blood supply causes the bone tissue to die. The condition is also known as avascular necrosis, meaning the compromised blood supply leads to tissue death, or bone infarction. Knee osteonecrosis mostly affects the elderly and women are three times more likely to develop knee osteoporosis than men.
In osteonecrosis, the lesion can affect the region beyond the growth plate of the bone (called epiphyseal plate) and can reach the next inner layer called the subchondral plate. If the lesion reaches the subchondral plate, the dying or necrotic segment of the bone may collapse. As a result, the joint line may disrupt and painful conditions (like secondary arthritis) develop.
Types
Knee osteonecrosis can be of two types – spontaneous or secondary.
Spontaneous osteonecrosis of the knee (SPONK)
- Usually affects one knee
- Symptoms are sudden onset of pain, increase in pain at night and upon lifting heavy objects and climbing stairs
- Does not affect other joints.
- Pain localized in affected area.
Secondary osteonecrosis
- Usually affects both knees.
- Intake of corticosteroids, alcohol, certain diseases (like systemic lupus erythematosus, caisson disease, sickle cell disease, and Gaucher disease), and metabolic conditions (like fat emboli, blood clot formation) increase the risk of developing secondary osteonecrosis.
- Affects other joints as well.
- Symptoms are of underlying disease. Prolonged pain is commonly seen.
- Pain is difficult to localize.
Spontaneous osteonecrosis of the knee (SPONK) affects people younger than 55 years; whereas secondary osteonecrosis is more common in elderly aged 55 years or more.
Location
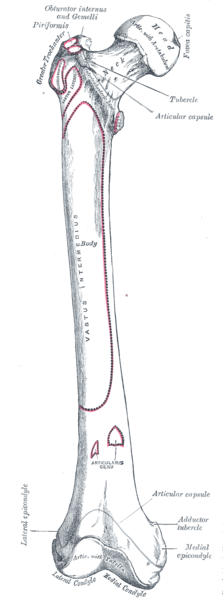
Osteonecrosis can affect any bone; however, it is more commonly seen in the hip and the knee. Knee osteonecrosis most commonly affects the medial condyle of the femur which is the ‘knobby’ part of the thigh bone on the inside of the knee. However, it can also affect the lateral condyle of the femur on the outside of the knee or the flat, top part of the lower leg bone called the tibial plateau.
Picture from Wikimedia Commons
Stages
Two arteries supply blood to the knee joint: the genicular artery and the popliteal artery. These two arteries may branch out and then reconnect at different points around the knees to maintain proper blood circulation. Problems with blood circulation may limit the supply to any of the bones of the joint, leading to osteonecrosis.
Knee osteonecrosis develops through following 4 stages:
- Stage I, in which pain and other symptoms are most intense.
- Stage II, in which the rounded edge of the thighbone starts to flatten out.
- Stage III, in which the bone begins to die and the outermost covering of the bones called articular cartilage begins to loosen.
- Stage IV, in which the bone begins to collapse.
Signs and Symptoms
Common symptoms of spontaneous osteonecrosis of the knee (SPONK) and secondary osteonecrosis may be listed as:
- Sudden pain on the inside of the knee
- Swelling all over the knee
- Pain triggered by some injury or a particular activity
- Increase in pain at night
- Increase in pain with activity
- Affected area painful to touch
- Limited motion of the knee joint due to pain
Causes and Risks
The exact cause of knee osteonecrosis is not known, however various factors might be playing a role in the development of the conditio. Such factors may include the following:
- Conditions that can change the blood supply to the bone (like a stress fracture or trauma)
- Build-up of fluid in the bone marrow cavity, which may put pressure on blood vessels and affect circulation adversely.
Factors like obesity, lupus, alcoholism, sickle cell anemia, kidney transplants, and use of steroids increase the risk of developing secondary knee osteonecrosis. However, no risk factors for spontaneous osteonecrosis of the knee (SPONK) have been identified.
Tests and Diagnosis
The following tests can be performed to diagnose knee osteonecrosis:
- X-ray scanning: Though the X-ray scan in stage I is normal; in stage II, the flattening of the rounded edge of femur can be seen. In stage III, the loosening of the articular cartilage and bone death can be seen. X-rays can also show the destruction of the articular cartilage and formation of bone spurs in stage IV.
- Magnetic resonance imaging (MRI) scan: MRI scans can detect the presence and extent of osteonecrosis earlier than an X-ray scan.
- Bone scans: Bone scans are better at diagnosing spontaneous osteonecrosis of the knee (SPONK). The bone scans may also show osteonecrotic lesions in the early stages of the disease itself.
Treatment
A multi-pronged approach to treating and managing osteonecrosis is necessary. The choice of treatment depends on severity of osteonecrosis.
Medications
Analgesics (painkillers) and non-steroidal anti-inflammatory drugs (NSAIDs) are prescribed for pain management. Overall medication is only useful in symptomatic relief and more so in spontaneous osteonecrosis rather than secondary osteonecrosis.
Devices
Clutches or braces may be worn, which relieve pressure from the joint surface.
Physical therapy
Physical exercises are recommended to strengthen the thigh muscles. Patients are advised to modify their activities to gain a better management of knee pain.
Surgery
Surgery is recommended in the cases where more than half of the bone surface is affected. Different surgical procedures include:
- Debridement or arthroscopic cleansing of the knee joint, in which loose parts of the cartilage and inflamed tissue are removed from the joint.
- Drilling and core decompression, which reduces pressure on the bone surface to restore blood circulation.
- Knee replacement
- Use of osteochondral grafts
- Osteotomy or removing part of tibial bone may be recommended to patients with spontaneous osteonecrosis of the knee (SPONK).
- Knee arthroplasty involves surgical repair of the knee joint, and is recommended in the late stages of the disease and for patients who do not respond to other treatments
Complications and Prognosis
Though treatment procedures like core decompression have minimal complications, they may still carry the risk of infection and fracture. Total knee arthroplasty on the other hand, is considered to be a safer and more effective option. However, it may also result in complications like nerve injury, infection, fracture, swelling, and dislocation of the kneecap (patella).
The prognosis of spontaneous osteonecrosis of the knee (SPONK) depends on the size of the lesion and worsens with advancement of the lesions. Prognosis of secondary osteonecrosis depends on stage and location of the lesion, and is not determined as much by size. As with most necrotic diseases, treatment depends on how soon the correct medical treatment is commenced.
References :
http://orthoinfo.aaos.org/topic.cfm?topic=a00225
http://emedicine.medscape.com/article/1252556-overview
http://www.hss.edu/conditions_osteonecrosis-of-the-knee-overview.asp