Pelvic Organ Prolapse (POP)
What is pelvic organ prolapse?
Pelvic organ prolapse refers to the condition characterized by an abnormal descent of female pelvic organs (the bladder, uterus, the small bowel and large bowel), due to which vagina and/or uterus protrude. A prolapse or slipping out of these organs from their normal anatomical position occurs with weakening of the tissues (muscles and ligaments) that normally hold up the pelvic organs in women. Vaginal child birth, advancing age, removal of uterus, or obesity may result in a prolapse.
The concern about the possibility of a prolapse later in life is one of the several reasons why some women opt for elective cesarean section (C-section) during childbirth. Many women, who have undergone childbirth, may have some degree of prolapse. However, most of the prolapses do not present with significant symptoms that compels a person to seek treatment.
How common is it?
The exact prevalence of pelvic organ prolapse is difficult to assess. As many as 25% women, who have children, may have a prolapse without showing the symptoms. However, less than 9% of such women require medical intervention for the condition.
Types of Prolapse
Pelvic organ prolapses can be of four types:
Cystocele
Also known as a dropped bladder, the protrusion involves the front portion of the vagina and bladder.
Rectocele
The back of the vagina and rectum are involved.
Enterocele
The upper portion of the vaginal wall and small bowel are involved.
Uterine prolapse
In this type, the uterus descends downward.
Location of Prolapse
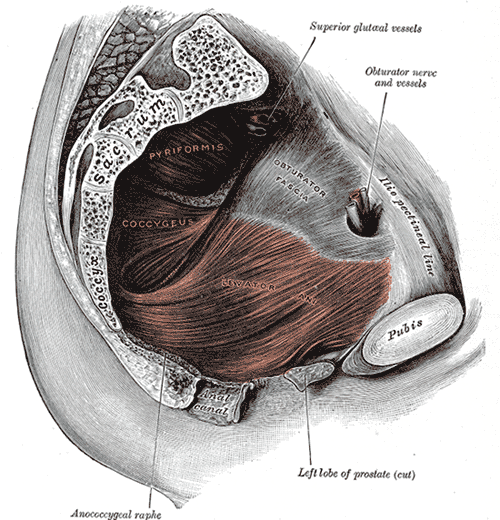
Pelvic organ prolapse involves pelvic organs which leave their normal position in the pelvis. The pelvic floor in humans acts as the lowest boundary, on which all the abdominal and pelvic organs rest. It acts like a sling made up of various muscles and ligaments, which are connected at the ends.
Picture of the pelvic floor from Wikimedia Commons
The vagina and the uterus are supported by some of the pelvis ligaments and muscles. Around the vagina, there are no muscles except the ones at its entrance (bulbocavernosus muscles). Another type of muscle called levator muscle passes around the vagina and the rectum. Levator muscle inserts into a structure called levator plate. Levator plate supports rectum, the vagina and the neck of the bladder.
A group of muscles called perineal body joins vagina and anus and maintains the integrity of the pelvic floor. Muscles called endopelvic fascia also provide support to the pelvis. Stretching and tearing of these muscles can lead to pelvic floor defects. Childbirth, aging and some other factors can result in extreme stretching and tearing of the involved muscles, resulting in a prolapse.
Signs and Symptoms
Symptoms of pelvic organ prolapse vary with the type and may include vaginal, urinary, bowel and sexual symptoms.
Vaginal symptoms
- Feeling a bulge
- Visible protrusion
- Heaviness or bearing down sensation
- Pressure
Urinary symptoms
- Increased frequency
- Increased urgency
- Incontinence or leaking of urine due to loss of control on involved muscles
- Hesitancy
- Prolonged or weak urinary stream
- Feeling of incomplete emptying of bladder
- Changing position to start or complete emptying of bladder
Bowel symptoms
- Incontinence of stool due to loss of control on involved muscles
- Feeling of incomplete emptying of rectum
- Straining during bowel movements
- Increased urgency
- Using fingers or pushing around the vagina to empty the rectum
Sexual symptoms
- Painful sexual intercourse (dyspareunia)
- Decreased sexual drive
Video Explanation
What causes a prolapse?
Stretching and tearing of pelvis muscles (like the endopelvic fascia, levator muscles, and perineal body) leads to pelvic floor defects. Pelvic organ prolapse may be caused by multiple defects, which may include the following :
- Childbirth (vaginal birth)
- Damage to the associated nerves (like partial pudendal neuropathy, perineal neuropathy, and diabetic neuropathy)
- Changes in genital organs (genital atrophy)
- Pelvic tumors
- Problems with sacral nerve
Risk Factors
Vaginal delivery, increasing age, and obesity are the main risk factors linked with a pelvic organ prolapse. Other factors that increase the risk of developing a prolapse are:
- Pregnancy (as the growing fetus puts pressure on pelvis)
- Delivery using forceps
- Young age at first delivery
- Prolonged labor (especially pushing phase)
- Excessive birth weight of infant (more than 9.9 pounds)
- Abnormalities in shape or orientation of pelvic bone
- Family history
- Conditions increasing pressure on abdomen and pelvis (such as obesity, constipation, smoking, chronic pulmonary disease, jobs involving lifting heavy objects)
- Abnormalities in connective tissue (like in Marfan disease)
- Surgical removal of uterus
- Estrogen deficiency
Tests and Diagnosis
A physical examination can reveal the strength of the pelvic floor tissue (muscles and of ligaments) that support the vaginal walls, rectum, uterus, urethra, and bladder.
An ultrasound can detect the defects in pelvic organs and their positions in pelvis. A magnetic resonance imaging (MRI) scan can provide detailed image of the pelvis.
Cystoscopy can be performed to evaluate symptoms of urinary frequency, urgency, or bladder pain.
Treatment
Treatment options for a prolapse include the following:
Physical therapy
Physical therapy helps in strengthening the pelvic floor muscles. Pelvic muscle exercises (PMEs) are often helpful in improving the tone of the muscles that constitute the pelvic floor.
Devices
A device called a pessary may be inserted into the vagina non-surgically. A pessary supports pelvic structures, relieves pressures on the bladder and bowel and thus, reduces prolapse inside the vagina. However, use of a pessary may lead to side-effects like vaginal discharge and odor.
Surgery
Surgery can be done vaginally, abdominally or laparoscopically.
- Reconstructive surgery can be performed to correct the prolapsed vagina. It is recommended in women who wish to maintain or improve vaginal sexual function.
- Obliterative surgery can be performed to closes off the vaginal canal in women who are no longer sexually active.
- Vaginal wall repair can be done in a procedure called colporrhaphy.
- With sacrocolpopexy, the upper part of vagina is suspended with a synthetic mesh.
- In vaginal approaches, the upper vagina or cervix can be attached to the existing ligament to provide extra support.
Medication
Estrogen replacement therapy (ERT) is recommended to some menopausal women, who have lower estrogen levels resulting in pelvic organ prolapse. ERT may strengthen the vaginal muscles in such cases.
Complications and Prognosis
Surgical procedures carry a risk of injuring the bladder, urethra (duct joining the bladder to urinary opening), and ureters (ducts joining the kidneys and the urinary bladder). Some surgeries might result into difficulty emptying the bladder completely. Sexual dysfunction is also seen in some cases after vaginal repair. Urinary incontinence may also start after surgeries.
Although the procedures for treating pelvic organ prolapse have fairly good success rate, the aforementioned complications may arise in some patients.
References :
http://emedicine.medscape.com/article/276259-overview
http://www.webmd.com/urinary-incontinence-oab/pelvic-organ-prolapse
http://www.mayoclinic.org/pelvic-organ-prolapse/treatment.html