Peroneal Nerve Location, Injury, Causes of Pain and Palsy
Overview
The peroneal nerve, also known as common fibular nerve, is one of the branches of the sciatic nerve. It is the most commonly injured nerve of the lower leg due to its location. Peroneal nerve injury and disease may arise due to various possible causes ranging from trauma, compression or infection. Apart from sensory symptoms such as pain, tingling and numbness with peroneal nerve disease there are other major motor symptoms since the peroneal nerve supplies the muscles that control the movement of the foot. These motor symptoms are known as foot drop.
The Peroneal Nerve
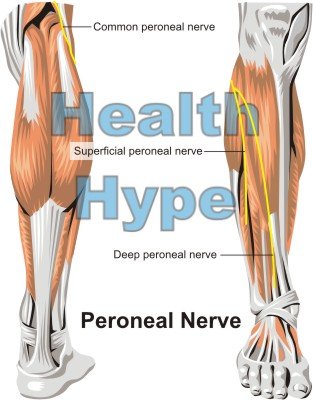
The peroneal nerve is the smaller terminal branch of the sciatic nerve, which arises from the lumbar and sacral spinal nerves (L4 to S2). The other terminal branch of the sciatic nerve which is much larger is the tibial nerve. It has two branches – superficial peroneal nerve and deep peroneal nerve. The proper term for the peroneal nerve before it terminates into the superficial and deep branches is the common peroneal nerve. It also gives off another branch which is known as the lateral sural cutaneous nerve.
Location of the Peroneal Nerve
- The peroneal nerve begins at the top of the popliteal fossa – the area at the back of the knee.
- It follows the inner (medial side) of the biceps femoris muscle and its tendon that is located at the upper outer (lateral) side of the popliteal fossa.
- The nerve then passes over (superficial) to the lateral head of the gastrocnemius muscle.
- From here it travels around the back (posterior aspect) of the head of the fibula.
- It then winds around the neck of the fibula and divides into the superficial and deep peroneal nerves.
Superficial Peroneal Nerve
- Supplies the lateral compartment of the leg.
- Innervates the fibularis longus and fibularis brevis muscles.
- Sensory fibers to the dorsum of the foot (top of the foot) except the web between the first and second toes.
Deep Peroneal Nerve
- Supplies the anterior compartment of the leg.
- Innervates the tibialis anterior, extensor digitorum longus, fibularis (peronæus) tertius, and extensor hallucis longus (propius), and the ankle joint.
- It divides into a lateral and medial branch.
- The lateral branch supplies the extensor digitorum brevis and the extensor hallucis brevis muscles.
- The medial branch supplies the skin of the web of toes between the first and second toes.
Lateral Sural Cutaneous Nerve
- Arises from the common peroneal nerve.
- It joins the medial sural cutaneous nerve which originates from the tibial nerve to form the sural nerve.
- Supplies the skin on the outer (lateral) and back (posterior) surfaces of the leg.
- Continues downwards to the foot where it is known as the lateral dorsal cutaneous nerve.
- Here it supplies the outer (lateral) side of the foot and little toe.
Muscle Movements
The muscles of the anterior and compartments of the leg, which are supplied by the peroneal nerve, are the dorsiflexors of the ankle and evertors of the foot. It mainly controls dorsiflexion and eversion of the foot but is also responsible for inversion of the foot and extension of the toes. The actions of these muscles are as follows :
- Dorsiflexion at the ankle is raising of the foot towards the leg.
- Eversion of the foot is moving the foot outwards once inverted so the the sole returns to facing downwards.
- Inversion is turning the foot inwards so that the sole of the foot faces sideways (inwards).
- Extension of the big toe or outer four toes can be controlled separately. This is where the toes curl upwards towards the top of the foot.
Peroneal Nerve Problems
Neuropathy is the term for any nerve disease or disorder. When it affects the nerves outside the brain and spinal cord it is known as peripheral neuropathy. If a single nerve is affected then it is referred to as a mononeuropathy or when several nerves are involved then it is known as polyneuropathy. The most common mononeuropathy in the lower limb (leg) involves the common peroneal nerve. Since the nerve has both a sensory (sensation) and motor (muscle movement) component, injury or disease of the peroneal nerve may lead to abnormal sensations (paresthesia), pain, muscle weakness or paralysis.
Peroneal nerve injury or disease may be associated with trauma or compression, infection, tumors or inflammatory disorders of the nerves or tissues in general. However, majority of the causes are related to trauma and compression of the nerve. Depending on the cause, the following may occur :
- demyelination – the insulating layer around the nerve wears out.
- nerve block (neurapraxia) – nerve impulses are not conducted despite there being no injury to the nerve sheath or fibers.
- axonal damage (axonotmesis) – the nerve fibers comprising of the axons is damaged but the nerve sheath is intact.
- severed nerved (neurotmesis) – partial or complete severance of the nerve.
Causes
There are a wide range of causes of peroneal nerve injury or disease. This includes :
- Leg crossing that applies constant pressure to the nerve.
- Trauma to the leg particularly around the area of the knee including blunt force trauma or penetrating injury.
- Surgery particularly knee surgery although it may occur with hip surgery where the sciatic nerve may be affected.
- Fracture of the lower leg bones especially the fibula.
- Repetitive strain injury to the leg with certain sports particularly when it involves kicking and with dancing.
- Sitting or lying down for prolonged periods which applies on the leg, especially around the knee.
- Knee problems such as dislocation, bicruciate injury and osteoarthritis.
- Ankle sprains that are severe or occur repeatedly.
- Plaster casts or braces that cause repetitive or prolonged pressure on the leg.
- Growths that cause compression on the nerve such as ganglionic cysts, schwannomas or lipomas.
- Stretch injury of the nerve with prolonged squatting or sudden stretching.
- Compartment syndrome where pressure within a compartment due to swelling or bleeding compresses the nerve.
Other causes may affect the sciatic nerve and therefore involve its branches or some conditions may not be specific to the peroneal nerve, such as generalized neuropathy.
Symptoms
Pain and Paresthesia
Pain and paresthesia are symptoms associated with the sensory component of the peroneal nerve. Paresthesia is the term for abnormal sensations such as “pins and needles”, tingling and numbness. It may precede the onset of pain in some cases. Paresthesias run along the course of the common peroneal nerve and its branches – the lateral aspect of the leg (outer side) and foot, top of the foot and webs of the toes.
Pain tends to be worse at the site of the nerve compression or injury but can run along its course. When the sciatic nerve is injured or compressed then pain or paresthesia may emanate from the lower back and buttock region, down the thigh to involve the lower leg and foot supplied by the peroneal and tibial nerves.
Weakness and Paralysis
Motor symptoms of peroneal neuropathy includes muscle weakness of varying degrees or flaccid paralysis of all the muscles in the anterior and lateral compartment of the leg should the nerve be cut (severed). Paresthesias (abnormal sensations) are also common with the muscle weakness or paralysis. When the peroneal nerve is injured or diseased, dorsiflexion and eversion of the foot are impaired. This condition is commonly referred to as foot drop where the foot is dragging when walking.
Foot drop is where a person cannot raise the foot and clear the toes from the ground thereby causing it to drag. Similarly the foot is not lowered to the ground in a controlled manner and slaps down hard once the heel touches the ground. The weakness and paralysis may be accompanied by muscle atropy over time where the muscle shrinks in size since it is not as active, if at all. People with muscle weakness or paralysis due to peroneal nerve injury or disease may attempt to compensate with one of the following gaits :
- High-stepping – a person bends more at the hip and knee joint to raise the affected leg higher than is necessary with each step.
- Waddling – a person leans more towards the unaffected leg and slightly raises the hip on the affected side to avoid leaning as much on the affected leg.
- Swing-out – a person swings the leg outwards (laterally) with each step to avoid the foot and toes from dragging on the ground.
References
1. Peroneal mononeuropathy. Emedicine Medscape
2. Peroneal nerve palsy. Duke’s Orthopaedics