Piriformis Syndrome
What is piriformis syndrome?
Piriformis syndrome is a rare condition characterized by pain, instability, tingling and numbness in the lower back, buttocks, lower thighs and the calves. It arises due to the irritation or compression of the sciatic nerve by the piriformis muscle during running or sitting. The longest and widest nerve of the body, the sciatic nerve is prone to a number of conditions that can lead to pain, numbness and tingling along its path.
Piriformis syndrome is just one of these conditions that affects the sciatic nerve along its pat to the lower leg. The symptoms may be experienced along the entire course of the the sciatic nerve or in specific areas supplied by this nerve like the skin of the leg, the muscles of the thigh, leg and foot on the back side.
How common is piriformis syndrome?
Exact incidence and frequency of piriformis syndrome is not known; however, different studies indicate the presence of pirifomis syndrome in 6% cases of patients suffering from lower back pain in the United States. This rare syndrome affects more females than males in a 6:1 ratio.
Location
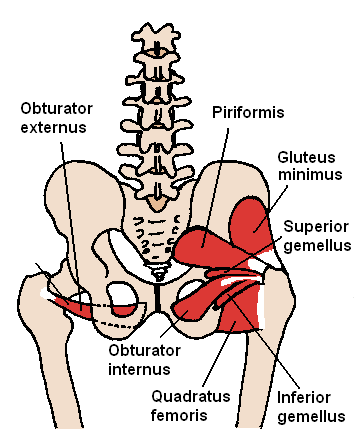
Simply, the piriformis muscle lies within the pelvis running from the front of the sacrum to the side of the femur. The sacrum is a collection of five fused vertebrae that lies approximately at the top of the buttock. Below it lies the tailbone – coccyx. The femur is the longest bone in the body commonly referred to as the thigh bone.
Picture from Wikimedia Commons
The sciatic nerve emerges from the lower back (L4 to S3) and travels through the buttock and down the back part of the lower limb and the foot. If along the course the sciatic nerve gets compressed by the piriformis muscle, it can cause instability and pain in the hip, tailbone (coccyx), buttock, groin, or foot. The sciatic nerve passes under the piriformis muscle.
Effects of Piriformis Syndrome
The sciatic nerve has two parts – the peroneal and tibial parts. These two parts of the sciatic nerve can emerge from the pelvis in 4 ways:
- both can pass in front of the piriformis,
- the peroneal part of the sciatic nerve can pass through the piriformis whereas the tibial part passes in front of the piriformis muscle,
- the peroneal part can make a loop above the back aspect of the piriformis muscle, whereas the tibial part passes in front of the piriformis muscle, or
- the entire sciatic nerve goes through the piriformis muscle.
Dysfunction, inflammation, or spasm of the piriformis muscle can cause piriformis syndrome. Piriformis syndrome is usually a result of blunt trauma to the buttocks. Apart from the ensuing inflammation, there may also be bleeding with subsequent clotting within the muscle as well as the release of various chemicals (like serotonin, prostaglandin E, bradykinin, and histamine) from blood cells. Less commonly, the sciatic nerve may become entrapped under the piriformis muscle due to an enlarged or inflamed piriformis muscle, cysts, tumors, or appearance of balloon-like structures in blood vessels (pseudoaneurysms) due to leaking of blood.
Signs and Symptoms
Patients with piriformis syndrome may show the following symptoms:
- Chronic pain in the buttocks and lower back
- Pain radiating to the lower leg
- Pain worsening with walking or squatting
- Pain increasing during bowel movements
- Pain in the outer vaginal folds (labia majora) in women
- Pain in the scrotum in men
- Painful sexual intercourse in women
- Pain during getting up from bed
- Pain increasing upon holding and rotating the hip
- Pain increasing upon sitting
- Pain increasing by lifting and reducing by traction on the affected leg
Causes and risk factors
Causes of piriformis syndrome may be grouped as:
- Trauma to the buttocks
- Sport injuries during skiing, tennis players
- Occupational jobs including driving for long periods
- Narrowed spinal canal (spinal stenosis)
- Anatomical changes in branching pattern of the sciatic nerve or in the piriformis muscle
Truck drivers and long-distance bikers are at increased risk of developing piriformis syndrome.
Sciatica vs Piriformis Syndrome
Tests and Diagnosis
The following tests can help in diagnosing piriformis syndrome:
- Physical examination: Feeling pain when thigh is flexed and rotated internally (Freiberg’s maneuver), when the affected leg is held in a sitting position (Pace’s maneuver), or when in the bent position, the patient’s buttocks are pressed on the point where the sciatic nerve crosses the piriformis muscle (Mirkin test) can diagnose piriformis syndrome.
- Imaging studies: A computed tomography (CT) scan may show a large mass in front of the piriformis muscle, narrowing of spinal canal, and arthritic changes. A magnetic resonance imaging (MRI) scan can detect the presence of other reasons (like herniated disc, abscess, or spinal tumor) that may be causing back pain.
- Electromyography (EMG): An electromyogram can determine neurologic or muscular damage. In piriformis syndrome, the EMG findings of piriformis muscles are abnormal.
- Reflex test: A reflex test called H-reflex checks the response of motor (movement-related) nerve fibers.
Treatment and Exercises
Treatment for piriformis syndrome includes physical therapy, occupational therapy, surgical intervention, and the use of medication. The treatment options differ depending on whether the patient is in injury phase, or recovery, or maintenance phase.
Injury phase
Treating acute pain of piriformis syndrome involves an extensive rehabilitation program, consisting of medical or surgical attention and physical and occupational therapy.
- Rest, avoiding offending activities and starting physical therapy is recommended.
- Physical therapy involves light and gradual stretching of the piriformis muscle after a brief warm-up session. Also, soft-tissue massage helps in decreasing tightness of the muscles and decreases irritation of the sciatic nerve.
- Flexing and extending the knees, taking a warm bath, and performing knee bends help immensely.
- Application of cold packs after exercise decreases pain and inflammation.
- Occupational therapy focuses on avoiding prolonged sitting.
- In rare cases some patients require surgical intervention, which may include release of the piriformis tendon.
- Non-steroidal anti-inflammatory medications (NSAIDs), injections of local anesthetics (like lidocaine, bupivacaine) and corticosteroids in the piriformis muscle, massage, and ultrasound treatment can help in decreasing pain.
– NSAIDs provide temporary pain relief.
– Corticosteroid injections are given near the point where the sciatic nerve crosses the piriformis muscle; however, these injections provide just temporary relief from pain.
Recovery phase
Physical therapy in this phase focuses on strengthening the piriformis muscles gradually.
Maintenance phase
In this phase, the physical therapy aims to increase flexibility and strength of the piriformis muscles. Patients are advised to change positions frequently to remove the source of pressure around the buttock. Activities that elicit pain (like running or bicycling) should be avoided till the piriformis muscle is strong enough.
Stretches Video
References :
http://www.webmd.com/pain-management/guide/piriformis-syndrome-causes-symptoms-treatments
http://emedicine.medscape.com/article/87545-overview
http://familydoctor.org/familydoctor/en/diseases-conditions/piriformis-syndrome.html