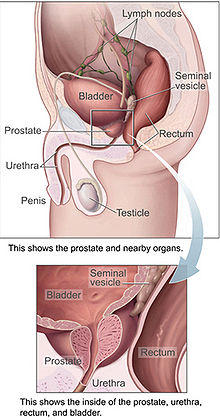
Prostate Cancer Diagnosis, Tests, Biopsy and Scans
Patients presenting with symptoms of prostate cancer would have reached a stage at which curative interventions are usually not possible since the symptoms are often only present in the advanced stages. Detection of prostate cancer prior to the onset of symptoms is therefore necessary for adopting a curative line of management. With aggressive screening measures and good public awareness these days, almost 70% to 80% of the prostate cancers are currently diagnosed in the early stages. The early diagnosis is partly responsible for the recent fall in the prostate cancer related mortality in the US.
One of the most important clinical examination for evaluation of a patient for prostate cancer is the DRE (digital rectal examination). Simple screening tests like PSA (prostate specific antigen) estimation are usually performed to detect any individual at high risk for developing prostate cancer. Additional diagnostic tests are considered in patients with enlarged prostate, elevated PSA value, urological symptoms, or family history of prostate cancer.
Digital Rectal Examination
DRE is a useful clinical examination but has a low sensitivity and specificity for diagnosis of prostate cancer. All suspected or abnormal DREs should be biopsied. A palpable nodule on DRE is one of the most common clinical finding that prompts biopsy leading to the diagnosis of prostate cancer. Other features may include a stony hard prostate with a loss of the median sulcus on the prostate gland.
PSA Screening and Diagnostic Tests
PSA screening tests include PSA levels, percent-free PSA, and PSA velocity values. The PSA level testing has a good sensitivity for prostrate cancer but has a low specificity as conditions like benign prostatic hypertrophy and prostatitis can show false-positive PSA elevations.
PSA level of more than 4 ng/mL is considered to be significant and has about 30% predictive value for prostate cancer (chance of detection of prostate cancer) at biopsy and 70 to 80% of tumors can be detected by this approach. The positive predictive value for PSA levels above 10 ng/mL increases to more than 60% for prostate cancer. More than 60% of prostate cancer patients are diagnosed when asymptomatic only because of the elevated PSA levels.
PSA velocity, percent-free PSA and PSA density are other PSA based screening tests.
The rate of change of PSA value over a period of time is referred as PSA velocity. Calculation of PSA velocity requires a minimum of 3 values of PSA levels collected over a period not less than 18 months. A PSA velocity value above 0.75 ng/mL per year is considered to be significant.
Percent-free PSA is the free PSA expressed as the ratio with total PSA. Men with prostate cancer have significantly lower percent-free PSA compared with men without prostate cancer. Percent-free PSA of less than 25% is considered to be clinically significant. The PSA density can be found by dividing the PSA value by the volume obtained with help of a trans-rectal ultrasound (TRUS).
Prostate Cancer Biopsy
A TRUS guided transrectal needle biopsy is performed to confirm diagnosis of prostate cancer in men :
- with a significant PSA based finding
- with an abnormal DRE
- whom prostate cancer is suspected
In a prostate biopsy, sextant biopsy specimens (base, midgland, and apex on each side) are usually obtained and in high risk patients seminal vesicles are also sampled. Other radiological studies as diagnostic aids for prostate cancer evaluation are usually employed when PSA levels above 10 ng/mL.
How many samples are taken in a prostate biopsy?
A sextant or 6-core biopsy scheme used to be the standard approach where 6 samples are taken systematically from the prostate. The 6 core samples included one each from the base, mid-gland, and apex on either side.
The currently recommended scheme for biopsy is the extended-pattern biopsy which involves taking 12 core samples systematically. In addition, further samples are taken from any lesion that is detected upon a digital rectal examination or ultrasound.
A saturation biopsy scheme (only when indicated) involves taking 30-50 core specimens. Seminal vesicles also may be included in the biopsy in some high risk patients.
What is done with the biopsy sample?
The tissue samples from the prostate biopsy are examined by a pathologist under a microscope for cancer cells.
If the biopsy sample reveals no cancerous cells, it could mean either the person does not have prostate cancer, or the prostate biopsy probably missed the tumor foci.
If the pathologist finds cancer cells, the next step is to find the Gleason score which is needed in grading the tumor. The relevance of this is discussed in detail under Cancer Staging and Grading.
Gleason grading evaluates the structural patterns of individual cancer glands. Five distinct patterns of growth are described. This includes well differentiated to poorly differentiated, with pattern 1 denoting the most differentiated, whereas pattern 5 stand for the most undifferentiated and with loss of the glandular architecture.
The final Gleason score is the sum of the grades of the most common, and second most common growth patterns. The total Gleason score can range from 2 to 10. The further management is planned based on the Gleason score.
Repeat Prostate Biopsy Tests
Patients with negative biopsy results are typically followed up conservatively with serial PSA levels and annual digital rectal examinations. A repeat biopsy is performed when PSA levels are persistently rising, if the initial biopsy is deemed inadequate or if DRE shows new nodularity or induration.
Complications of Prostate Biopsy
Bleeding
Patients undergoing transrectal prostate biopsy may pass some blood through the rectum (hematochezia) and in the urine (hematuria) for a few days after the procedure. Some blood in semen (hematospermia) for 2-3 weeks (less frequently up to 1-2 months) may be noticed.
Pain and Discomfort
Pain is usually minimal in patients who have anesthesia for the prostate biopsy procedure. The patients who undergo transperineal biopsy may experience some tenderness over the area of the procedure for few days. Pain and tenderness is more common in saturation biopsy requiring analgesics for about a week. Avoiding stress and straining immediately after the procedure will reduce the associated unpleasant feelings.
Infections
Serious infections like septicemia or an abscess are infrequent when proper sterile precautions are observed and with preventive antibiotic treatment. Infections are associated with increasing pain and tenderness or a high fever.
Urinary retention
Inability to pass urine (common in saturation biopsy) may require the insertion of a catheter till the inflammation leading to the retention subsides but most of the time it is self-limiting.
Warning Signs
High fever, excessive bleeding, increasing pain and tenderness, or inability to urinate after the procedure, should be immediately reported to the urologist.
Can prostate biopsy spread the tumor?
Theoretically cancer cells can spread through the biopsy needle tract. When there is a long tract for the needle to pass through from skin to the biopsy site, it would also mean that there is a long way back from the tumor to the skin surface. Such biopsies have higher chances for the cancer cells to drop off the needle and grow along the needle tract.
The needle tract for a transrectal prostate biopsy is extremely short since the biopsy needle goes through the rectal wall directly into the prostate. The chances of such spread is therefore extremely low. A remote risk of tumor spread may be attributed to the transperineal type of prostate biopsy, which is not a method that is commonly used these days. All patients in such reported instances of transperineal needle track spread had advanced stages prostatic cancer and Gleason score was high at the time of biopsy.
Overall reports of cancer spread due to a prostate biopsy appear to be highly exaggerated. A prostate biopsy is an integral tool in identifying, assessing and managing prostate cancer. The benefits of this procedure should always be taken into consideration before refusing the biopsy due to unfounded claims.
Radiology and Imaging Investigations
Transrectal Ultrasound (TRUS)
TRUS is the most important radiological investigation for the initial assessment of prostate cancer. Urologists use TRUS for guiding the needles in guided-biopsy. TRUS is also of use in prostate volume assessment and calculation of the PSA density. It is however not useful in assessing the involvement of the prostate capsule or the early extensions beyond the capsule. Use of Color duplex and power Doppler may help in specifically identifying the hypervascular areas that corresponds to the malignant lesions.
Computerized Tomography (CT Scan)
Prostate cancer evaluation often includes CT scan of the pelvis but its role is mostly limited to detection of lymph node metastases. The usefulness of CT scan in the detection of tumors confined to prostate tissue and quantification of extracapsular prostatic tumor is limited.
Magnetic Resonance Imaging (MRI)
MRI provides scope for assessment for extracapsular extension with better visualization of the prostatic capsule and provides a more detailed anatomic picture. The inclusion of MR spectroscopy improves the ability of MRI to localize prostatic cancer more accurately.
Bone Scan
Radionuclide bone scan is considered to be the standard investigation to evaluate high-risk patients for the presence of bone metastases. It is not recommended for low-risk patients. Patients with PSA levels of less than 10 ng/mL have only minimal chance for a positive bone scan, while patients having PSA levels above 50 ng/mL have a 50% chance of positive bone scan. Response to treatment in advanced prostate cancer can also be assessed with bone scans.
Positron Emission Tomography (PET)
The introduction of new tracers (like C11 choline) in PET imaging has been found to significantly enhance its use to detect intraprostatic disease and metastases to lymph nodes.
ProstaScint Scanning
Prostascint scanning utilizes monoclonal antibodies conjugated with radioisotopes to assess relapse of prostate cancer in patients with elevated PSA levels after primary therapy.
Last updated on September 11, 2018.





