Rabbit Fever (Tularemia)
What is rabbit fever?
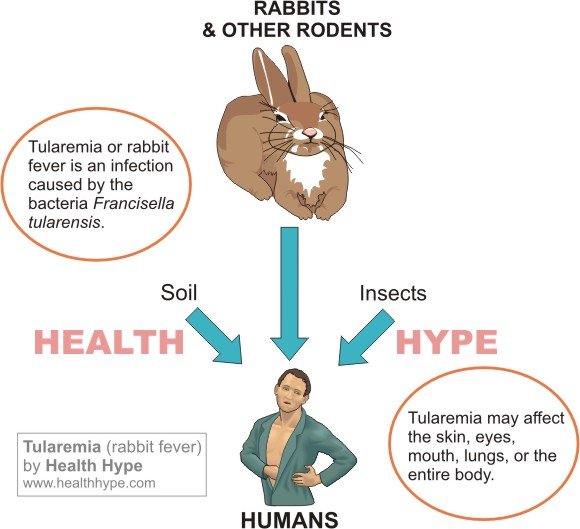
Rabbit fever, medically known as tularemia, is an infection with the bacteria Francisella tularensis. This infection mainly occurs in rodents, such as rabbits, squirrels and hares, hence the term ‘rabbit fever’. However, it can also affect fish, reptiles and humans. It is an acute infection and once a person recovers from it they will usually have lifelong immunity, although there can be relapses of the initial infection. Overall rabbit fever is a rare infection with only a few hundred cases seen in the United States every year. It is treatable and only a small percentage may lead to death as a result of the complications of untreated rabbit fever.
Rabbit fever disease
There are two types of rabbit fever bacteria – Francisella tularensis type A and type B. The more common type to infect humans is type A. It only occurs in rabbits and other rodents and is then transmitted to humans. Type B may be seen in reptiles and amphibians and can also infect humans although it is less frequent. There are several ways in which a person can be infected. Iit may cause several different types of presentations based on the way it infect the person.
Rabbit fever spread
The rabbit fever bacteria can enter the body through three ways :
- Mouth – orally
- Skin – intradermally
- Airways – inhalation
Mouth and eyes
Contact with the lining of the mouth or the eyes (conjunctiva) may also cause rabbit fever infection. It is a less common mode of transmission. It is more likely to occur with the hands making contact with infected material and then touching the eyes or mouth. Contaminated water and undercooked infected meat may also be a less frequent route of transmission.
Skin contact and insect bites
One of the more common ways for Francisella tularensis to enter the body is through the skin. It is believed that this bacteria can penetrate intact skin which is uncommon for most types of bacteria. A break in the skin will obviously be a more likely entry point. Therefore a person in direct contact with the infected tissues can contract the infection. Another common way through the skin is by the way of vectors. This means that some other biological entity carries the infection from the animal to human. In the case of rabbit fever it may be insects and in particular a tick bite.
Airways and lungs
The rabbit fever bacteria can be inhaled and then infect the airways and lungs. This may be seen with people who are in contact with soil containing the bacteria. It may also reach the lungs through the bloodstream from another site of infection. Contact with infected animal tissue may be a factor although it is more likely in people who are in close contact with rabbits. Human to human transmission has not been reported as yet.
Tularemia Types
There are several different ways in which tularemia may present. It can affect certain organs, cause only some symptoms in particular areas of the body and lead to different types of complications. This is largely dependent on how the tularemia bacteria is contracted. The two most common types of tularemia are :
Ulceroglandular tularemia
- Most common type.
- Lesions on hand and fingers.
- Swollen and tender lymph nodes in the area.
- Mainly by skin contact with the bacteria and insect bits.
Typhoidal tularemia
- This is also a common type of tularemia.
- Symptoms similar to typhoid fever.
- No localized symptoms at site of infection.
- Potentially fatal if left untreated.
Less common types of tularemia include :
Oculoglandular tularemia
- Uncommon type of tularemia.
- Eye symptoms similar to conjuctivitis (pink eye).
- Swollen and tender lymph nodes on affected side.
- Often spread by touching the eye with a contaminated hand.
Pneumonia tularemia
- This is also an uncommon type of tularemia.
- May occur with inhaling the bacteria of spread to lung in typhoidal tularemia.
- Symptoms typical of pneumonia.
- Also potentially fatal if left untreated.
Rare types of tularemia are often not discussed as tularemia on its own is rare and these presentations are almost never seen. It includes :
Glandular tularemia
- Swollen lymph nodes in one area.
- Similar to ulceroglandular tularemia without skin symptoms.
- Possibly caused by ingesting contaminated food and water.
Oropharyngeal tularemia
- Most likely due to consuming contaminated food and water.
- Swollen lymph nodes in the neck.
- Sore throat.
Septicemic tularemia
- Systemic illness like typhoidal tularemia but very severe.
- Acute respiratory distress syndrome (ARDS)
- Low blood pressure (hypotension)
- Multi-organ dysfunction.
Rabbit fever causes
Rabbit fever is caused by the bacterium Francisella tularensis.The modes of spread have been discussed above. Rabbit fever is more likely to occur with :
- Insect bites – ticks, deer flies and horse flies.
- Touching dead or sick animals, particularly rodents.
- Consuming contaminated food and water.
- Inhaling soil particles and or even small particles of infected tissue.
Risk factors for rabbit fever
Human to human spread does not occur so there is almost always some type of contact with the animal, its tissues or areas where it lives and breeds. People who are at a greater risk of contracting rabbit fever include :
- Hunters
- Butchers
- Fur farmers
- Veterinary workers
- Gardeners
- Wildlife workers and conservationists
- Laboratory workers
Rabbit fever symptoms
Rabbit fever symptoms are not unique and therefore is common for it to be misdiagnosed. It is important to consider a person’s medical history when considering the symptoms. The incubation period varies between 1 to 10 days but is typically between 2 to 4 days. This means that on average about 2 to 4 days passes from the time of infection until the first symptoms are seen.
Common symptoms among the different types of tularemia includes :
- Fever
- Chills
- Exhaustion
- Vomiting
- Diarrhea
- Swollen lymph nodes (localized or generalized)
 Picture of tularemia skin ulcer from Wikimedia Commons
Picture of tularemia skin ulcer from Wikimedia Commons
More specific symptoms include :
- Skin ulcers (ulceroglandular)
- Eye redness and pain, swollen eye and eyelid ulcers (oculoglandular)
- Cough, chest pain and difficulty breathingn (pneumonia)
- Sore throat (oropharyngeal)
- Enlarged spleen and/or liver with respiratory symptoms (typhoidal)
Rabbit fever diagnosis
Tularemia is not easy to diagnose and it is not uncommon for the diagnosis to be initially missed. The symptoms along with a history revealing possible contact with the animal may raise the suspicion of tularemia. Common blood tests like a complete blood count (CBC) may indicate an infection but does not specify the type of infection. More common infections may therefore be suspected initially. Even imaging studies like a chest X-ray may reveal pneumonia but not the cause of pneumonia. More specific tests will include :
- Culture where a blood or sputum sample is take and the bacteria grown in the laboratory to identify the species.
- Antibodies in the blood may be more specific for tularemia although it may not be detectable in the early stages.
 Picture of Francisella tularensis culture from Wikimedia Commons
Picture of Francisella tularensis culture from Wikimedia Commons
Rabbit fever treatment
Tularemia is treatable. It should not be left untreated as it is more likely to lead to complications some of which are fatal. Antibiotics are the drugs that can eradicate the infection although Francisella tularensis bacteria are resistant to penicillins and first-generation cephalosporins. Surgery is not necessary although large abscesses may need to be drained or severely infected skin may be debrided.
Medication
The antibiotic of choice is streptomycin. Other antibiotics that may be used include chloramphenicol especially if there is symptoms of meningitis and it may be combined with tetracycline. Alternatives to streptomycin include gentamicin, doxycycline and ciprofloxacin. However, the relapse rates are high with any antibiotic other than streptomycin.
References :