Subacute Thyroiditis (Temporary Thyroid Dysfunction)
What is subacute thyroiditis?
Subacute thyroiditis is a condition where the thyroid gland is inflamed for short periods of time leading to overactivity, then underactivity and eventually returning to a normal state. The condition responds spontaneously meaning that it heals on its own although medication may be used to limit the severity of the diseases and control the symptoms. There are three main types of subacute thyroiditis which are either caused by a virus or by the immune system attacking the thyroid gland (autoimmune). In a minority of cases there may be permanent damage to the thyroid gland leading to lifelong underactivity of the thyroid gland (hypothyroidism). However, the term subacute means that the thyroid dysfunction lasts for months or even a year but almost always returns to normal on its own. It is therefore not chronic.
Subacute Thyroiditis Effects
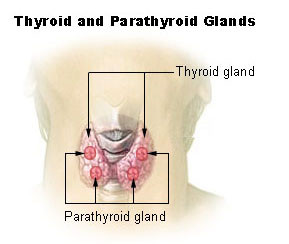
The thyroid gland is a medium sized gland sitting in the front of the neck. It has a right and left lobe joined by an isthmus. It secretes thyroid hormones which have a host of effects but primarily control the metabolism – the rate at which energy is produced. There are two thyroid hormones – triiodothyronine (T3) and thyroxine (T4) These hormones are stored in an inactive state within thyroid follicles. When needed, the pituitary gland secretes thyroid-stimulating hormone (TSH) which then acts on the thyroid gland. The thyroid hormones are then separated from storage proteins and released into the bloodstream.
Picture from Wikimedia Commons
Subacute Thyroiditis Hyperthyroidism
Inflammation of the thyroid gland has different effects. Subacute thyroiditis is one type of thyroid inflammation where both disordered thyroid states are seen. First the gland becomes overactive due to the inflammation. Higher than normal levels of thyroid hormones are secreted into the blood stream. This states of the thyroid gland is known as hyperthyroidism or thyrotoxicosis, the latter referring to the high levels of thyroid hormones in the bloodstream.
Subacute Thyroiditis Hypothyroidism
During hyperthyroidism, the thyroid hormone stores are depleted yet new thyroid hormones are not synthesized. Once these thyroid hormones are depleted, the levels in the bloodstream are lower than normal. The thyroid gland is said to be underactive and this is known as hypothyroidism. It is only a transient stage and may not be present in every case of subacute thyroiditis. However, sometimes this underactive state can be permanent if the thyroid gland is irreversibly damaged.
Subacute Thyroiditis Euthyroidism
Eventually the thyroid gland function returns to normal. This is known as euthyroidism. About 90% to 95% of subacute thyroidism patients will find the thyroid function returning to normal. It occurs on its own within weeks or months even if no treatment is commenced. Since most cases of subacute thyroiditis eventually results in normal thyroid function without the need for treatment, the condition is said to be self limiting.
Subacute Thyroiditis Types
There are three types of subacute thyroiditis classified according to the cellular changes in the thyroid gland, the cause or risk factor for its development. This includes :
- Subacute granulomatous thyroiditis
- Subacute lymphocytic thyroiditis
- Subacute post-partum thyroiditis
Subacute granulomatous thyroiditis
This type of thyroiditis is also known as subacute painful thyroiditis or de Quervain thyroiditis. Inflammation is a result of a virus directly damaging the thyroid gland or the action of the immune system directed at the viral protein in the thyroid gland. The immune system in this type of thyroiditis does not specifically target and attack the thyroid cells. Therefore it is not an autoimmune disease. There is the formation of a mass of tissue known as a granuloma which is typical of an infection, hence the name granulomatous thyroiditis.
Subacute lymphocytic thyroiditis
Subacute lymphocytic thyroiditis is also known as painless thyroiditis. The inflammation is a result of the immune system attacking the thyroid gland and is therefore an autoimmune disease. Large amounts of lymphocytes invade the thyroid gland tissue hence the name lymphocytic thyroiditis. While it seems to be a largely genetic disorder, it is also closely associated with the use of certain medication. Lymphocytic thyroiditis is more likely to lead to permanent hypothyroidism that subacute granulomatous thyroiditis.
Subacute post-partum thyroiditis
Subacute post-partum thyroiditis is inflammation of the thyroid gland associated with pregnancy. Changes in immune functioning leads to the immune system attacking the thyroid gland tissue.. It is autoimmune in nature as is the case with lymphocytic thyroiditis. The thyroid gland tissue shows a large amount of lymphocytes infiltrating it. Antibodies against the thyroid gland may form and this makes it more likely than the thyroid dysfunction will become permanent. The antibodies may be evident even before pregnancy or during pregnancy but the condition only becomes apparent a few months after giving birth.
Subacute Thyroiditis Causes
The causes may vary depending on the the type of subacute thyroiditis.
- Viral infections may cause subacute granulomatous thyroiditis and this includes viruses such as :
– Adenovirus
– Coxsackie virus
– Influenza
– Mumps
- Genetic factors which may play a role in all types of subacute thyroiditis.
- Medication use has been implicated in subacute lymphocytic thyroiditis and this includes drugs such as :
– Amiodarone
– Interferon-alpha
– Interleukin-2
– Lithium - Antibodies and changes in immune activity, like with the T-cells, are the cause of post-partum thyroiditis and may be related to the physiological changes with pregnancy and underlying genetic factors. This is similar to Hashimoto’s thyroiditis.
- Cigarette smoking increases the risk of post-partum thyroiditis.
- Idiopathic where there is no specific cause that has been identified for the type of subacute thyroiditis.
Subacute Thyroiditis Symptoms
The signs and symptoms of subacute thyroiditis largely depends on the type of thyroid gland dysfunction. Initially there is hyperthyroidism so the symptoms of thyroid gland overactivity are evident. Later this is followed by hypothyroidism and the symptoms of an underactive thyroid gland can be seen. Eventually thyroid gland function will return to normal in most cases and all symptoms gradually resolve.
Subacute Thyroiditis Overactive Thyroid Gland
- Anxiety, irritability and/or nervousness
- Excitable and hyperactive (sometimes)
- Intolerance to heat
- Weight loss
- Rapid heart rate
- Tremor
- Sweating
- Diarrhea
- Increased appetite
- Difficulty sleeping
- Fatigue
- Muscle weakness
Subacute Thyroiditis Underactive Thyroid Gland
- Depression
- Slow and sluggish demeanor
- Intolerance to cold
- Weight gain
- Puffy face
- Pale and dry skin
- Brittle hair and fingernails
- Hoarse voice
- Constipation
- Joint symptoms
- Fatigue
- Muscle weakness
- Excessive sleepiness
Differences in Subacute Thyroiditis Symptoms
There are some signs and symptoms that are more likely in certain type of subacute thyroiditis.
- Subacute granulomatous thyroiditis :
– Fever, fatigue and other flu-like symptoms.
– Neck pain, tenderness and painful swallowing.
– Muscle aches.
– Jaw and ear pain.
- Subacute lymphocytic thyroiditis :
– Painless enlargement of the thyroid gland (goiter).
– Lack of symptoms of an infection either during or before the onset of thyroiditis.
– Similar to Grave’s disease in presentation.
- Subacute post-partum thyroiditis :
– Firm enlargement of the thyroid gland which is painless.
– Pregnancy is the differentiating factor from subacute lymphocytic thyroiditis before tests are conducted.
– Similar to Grave’s disease in presentation.
Picture of eye symptoms in Grave’s disease from Wikimedia Commons.
Subacute Thyroiditis Diagnosis
The clinical presentation along with medical history should lead to a differential diagnosis of subacute thyroiditis. This can be further confirmed with blood tests, radioactive iodine imaging studies and a biopsy. A thyroid ultrasound may be conducted to exclude other thyroid diseases but cannot specifically indicate subacute thyroiditis.
Blood Tests for Subacute Thyroiditis
- Thyroid hormones – free T4 and T3
- Thyroid stimulating hormone (TSH)
- Thyroid antibodies
- Erythrocyte sedimentation rate (ESR) for infections.
Radioactive Iodine Uptake
Nuclear scintigraphy will allow for the uptake of radioactive iodine into the thyroid gland to be visualized. Typically there is a lower than normal uptake of iodine in subacute thyroiditis.
Picture of the images acquired through radioactive iodine and thyroid scintigraphy from Wikimedia Commons.
Thyroid Biopsy
Fine needle aspiration (FNA) allows for a collection of a small sample from the thyroid gland which can the be examined microscopically.
Subacute Thyroiditis Treatment
No thyroid-specific treatment is required for subacute thyroiditis of any type. The condition resolves on its own within months or even up to a year and thyroid function returns to normal. However, the following medication may be used is there is significant discomfort with thyroid gland enlargement or if the diseases is severe and persisting for a long time.
- NSAIDs – non-steroidal anti-inflammatory drugs
- Corticosteroids
Synthetic thyroid hormones may be considered if the thyroid dysfunction is prolonged and severe as well as if there is permanent hypothyroidism which is uncommon with subacute thyroiditis.
Subacute Thyroiditis Prevention
There is no specific preventative measure for subacute thyroiditis as most patients are not aware of the risk and even when risk factors are present it is not a common disorder. Women in the reproductive years who are planning to conceive should be cautious about cigarette smoking which appears to be a risk factor for subacute post-partum thyroiditis.
Subacute Thyroiditis Complications
The only significant complication is permanent hypothyroidism. Should this arise then the complications of hypothyroidism need to be considered. Therefore treatment with synthetic thyroid hormones are necessary in permanent hypothyroidism as well as to control the symptoms of the underactive thyroid gland.
References :