Trachea (Location, Functions) and Tracheal Deviation (Causes of Shift)
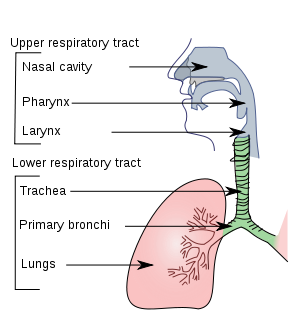
The trachea is the part of the respiratory tract that leads from the larynx and ends lower down in the thoracic cavity where it divides into the two main bronchi (left and right). It lies almost exactly in the middle of the neck (median) although in most healthy people, it may be noticed sitting slightly to the right. It runs down into the chest (thoracic) cavity, behind the breastbone, and diverges into the two bronchi at around the sternal angle.
Location of the Trachea
The trachea starts where the larynx ends – at the level of the C6 vertebra – and run down the middle of the neck anterior to the esophagus. Tracheal deviation, where the trachea shifts from this middle position (media plan) indicates some disease of the respiratory system or thoracic cavity. The trachea ends around the level of the T4 to T5 vertebrae. The point where it terminates also correlates with the sternal angle – the junction of the manubrium and body of the sternum (breastbone).
Anatomy of the Trachea
The trachea is a fibrocartilaginous tube. It is lined with ciliated respiratory epithelium and has incomplete C-shaped tracheal rings to prevent the trachea from collapsing. The gaps between the two ends of the C-shaped rings, which lies at the posterior part of the trachea, are joined by the trachealis muscle. This makes the posterior part of the trachea flat compare to the rounder front (anterior) and sides (lateral).
Functions of the Trachea
- The primary function of the trachea is to allow air to pass between the larynx and bronchi. It allows the air to be divided and routed into both lungs by terminating into the two main bronchi.
- The ciliated respiratory epithelium also traps dust particles in the air and propels it out of the respiratory passages, towards the pharynx (throat).
- The trachealis muscle that joins the two ends of the tracheal ring can contract thereby constricting the tracheal tube. This is useful for increasing the pressure during coughing to evacuate any irritants more effectively.
What is a tracheal deviation?
Windpipe Shift
Upon physical examination, a tracheal deviation may be detected. This means that the trachea (windpipe) has shifted more towards one side, either left or right. Any midline shift of the trachea should be investigated further for the cause, however, it should be noted other signs and symptoms will also be evident.
How is a tracheal deviation detected?
Respiratory Examination for Windpipe Shift
With the head facing to the front (anteriorly), the right index finger is placed on the suprasternal notch. This is the groove that sits on top of the manubrium of the sternum (breastbone) and can be easily palpated. Deeper palpation is necessary to pinpoint the trachea and this can be uncomfortable but should not be painful. Any pain at this point should be noted. The finger will follow the trachea up the neck as gently as possible.
While a tracheal deviation is a significant clinical finding, it should not be the sole factor for the diagnosis of any condition. Medical history, the results of diagnostic investigations and other signs and symptoms are necessary for a final diagnosis.
Common signs and symptoms associated with most of the causes of tracheal deviation include :
- Difficulty breathing (dyspnea)
- Cough
- Abnormal breathing sounds
Causes of Tracheal Deviation
Tracheal deviation does not only indicate pathology of the trachea itself. Any shift of the mediastinum, particularly the upper mediastinum, will result in a tracheal deviation. The mediastinum is the compartment in the center of the chest cavity, which also houses the heart and major blood vessels, and is surrounded on the left and right by the pleural cavity containing the lungs.
Tracheal shift towards lung problem
In diseased states where the pressure within the pleural cavity decreases on one side, the upper mediastinum (including the trachea) shifts towards the affected side.
- Atelectasis
- Also known as a collapsed lung, atelectasis refers to the diminished lung volume either as a result of a blockage (obstructive) or inability to inflate sufficiently.
- Pleural fibrosis
- Thickening of the pleura usually as a result of prolonged inflammation. Calcification may occur.
- Pneumonectomy
- Partial or complete surgical removal of the lung often conducted in order to treat lung cancer.
- Lung agenesis/aplasia
- Congenital abnormality where there is an absence of a lung and/or its bronchus.
The diseases above prevent the lung pressure from increasing due to inspiration or keep the lung pressure low even during expiration. Since the lung on the opposite side is functioning normally or to a greater degree than the affected side, the trachea will shift towards the diseased low-pressure side.
Tracheal shift away from the lung problem
In diseased states where the pressure within the pleural cavity increases on one side, the mediastinum (including the trachea) shifts away from the affected side.
- Pneumothoras
- Partial or complete collapse of the lung due to air entering the pleural space and compressing the lung thereby preventing it from expanding upon inspiration. Tracheal deviation more prominent in a tension pneumothorax.
- Pleural effusion
- Accumulation of fluid in the pleural space, which is the the area between the lung and chest wall. Significant clinical features like a tracheal deviation will only be present in the case of a massive pleural effusion.
- Tumors
- Any large mass of the bronchi, lung or pleural cavity including a benign or malignant tumor, may result in tracheal deviation.
Other causes
- Retrosternal goiter – enlargement of the thyroid gland or a portion of it lying behind the sternum as in the case of a multinodular goiter with retrosternal extension.
- Tracheal tumor
- Lung cancer
- Lymphoma or other causes of an extremely swollen neck lymph nodes
- Kyphoscoliosis


