Trigeminal Neuralgia (Nerve Face Pain)
What is Trigeminal Neuralgia?
Trigeminal neuralgia is defined as a painful condition involving irritation and inflammation of the trigeminal nerve. Trigeminal nerve carries sensation from the face to the brain. Trigeminal neuralgia, also called tic douloureux, causes unbearable facial pain on one side. Even the mildest activities can trigger this pain.
Trigeminal neuralgia starts with shorter, milder attacks but it soon changes into longer and frequent episodes of severe pain. The extent of pain is known to drive patients to the brink of suicide. The pain starts from trigeminal nerve and then spreads to the upper and lower jaws of one side of face. The pain may also cause a tic (facial spasm).
How Common is Trigeminal Neuralgia
Trigeminal neuralgia affects 3 out of every 20,000 people. In the US alone, nearly 15,000 cases are reported every year. Trigeminal neuralgia is more likely to occur in women than men, and it usually affects elderly or people over 50. The condition is often associated with multiple sclerosis. Nearly 1% to 2% of patients with one disease develop the other condition. Patients with both conditions often have facial pain on both sides. Apart from multiple sclerosis, hypertension (high blood pressure) is a known risk factor for this syndrome. Given the prevalence of hypertension across the globe, this may also impact on the incidence of trigeminal neuralgia.
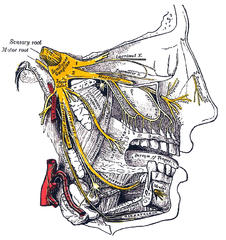
Picture of the trigeminal nerve anatomy from Wikimedia Commons
What Happens in Trigeminal Neuralgia?
The exact pathophysiology of trigeminal neuralgia is not clear. The trigeminal nerve is a sensory nerve that carries sensations like touch and pain from the face to the brain. It is one of 12 pairs of cranial nerves that arise directly from the brain without communicating via the spinal cord. As a sensory nerve, factors like damage and increased pressure on the nerve can result in pain.
The nerves have a protective covering called myelin, which is an insulator that also helps with the passage of nerve impulses. Loss of myelin (demyelination) can cause irregularities in the transmission of information. In some cases, it can amplify the sensory inputs. In such scenario, even the smallest stimuli can result in too much sensation. In trigeminal neuralgia, for example, a vibration can trigger an attack.
Trigeminal Neuralgia Location
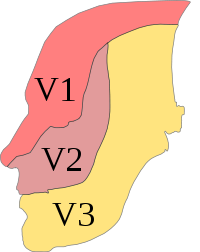
The trigeminal nerve is the fifth cranial nerve (CN V) and has three major branches :
- V1 – opthalmic branch
- V2 – maxillary branch
- V3 – mandibular branch
The opthalmic branch of the trigeminal nerve supplies the scalp, forehead, upper eyelid and nose. The maxillary branch supplies the cheek, lower eyelid, and outer rim of the openings to the nose (nares). The mandibular branch supplies the lower lip, chin, jaw and parts of the outer ear.
Picture of the trigeminal nerve branches from Wikimedia Commons
Therefore symptoms may be more prominent in these areas depending on which branch of the trigeminal nerve is affected. Usually only one trigeminal nerve is affected although both sides can be affected simultaneously. The maxillary and mandibular branches are the most commonly affected therefore the symptoms are mainly located in the regions supplied by these branches. For some unknown reason, the right side of the face is more frequently affected than the left.
Signs and Symptoms
Symptoms of trigeminal neuralgia may include the following:
- Irregular pangs of mild pain or severe jabbing or shooting pain
- Sensation of electric shock-like pain on specific locations
- Sudden attacks of pain triggered by routine actions like rubbing the face, shaving, talking, chewing, smiling, or drinking cold or hot drinks, touching, blowing the nose, brushing teeth, or facing cold air
- Attacks of pain lasting for few seconds
- Frequent episodes over days, weeks, or months or longer with periods of no pain in between
- Pain affecting the cheeks, jaws, gums, teeth, lips, or forehead
- Pain affecting one side of the face
- Focal or radiating pain
Attacks increase in frequency and intensity over time. There are contortions of the face of expressions during an attack. During attacks, patients may frown, grimace, or make sudden head movement to bear the pain – this results in tics.
Causes of Trigeminal Neuralgia
- In trigeminal neuralgia, a blood vessel at the base of the brain may exert pressure on the trigeminal nerve. This pressure disturbs the function of the nerve.
- Trigeminal neuralgia can be related to multiple sclerosis or can occur as a result of aging.
- It has a strong association with hypertension (high blood pressure).
- Disorders that damage the myelin sheath, inflammation of meninges (membranes covering the brain), or tumors compressing the trigeminal nerve may also cause trigeminal neuralgia.
- In many cases, however, a cause cannot be found.
Trigeminal Neuralgia Complications
Prolonged use of anticonvulsants or anti-spasm medicines for treating trigeminal neuralgia can produce side-effects and toxicity. Over years the medicines may also become less and less effective. In such cases a new anticonvulsant is prescribed, which may inadvertently produce more side-effects.
Surgery to treat trigeminal neuralgia may damage nearby nerves. This can cause conditions like anesthesia dolorosa or facial dysesthesia. Anesthesia dolorosa is a non-reversible condition, which causes pain and numbness in face. Facial dysesthesia involves unpleasant abnormal sensation.
Trigeminal neuralgia can cause depression and may affect quality of life in patients. In severe cases, the pain may lead to suicide.
Diagnosis of Trigeminal Neuralgia
A description of the pain may help diagnose trigeminal neuralgia. The description involves the information about type of the pain, location in the face and the triggers. Various tests used for diagnosing trigeminal neuralgia may include the following:
- Neurological examinations give information about the location of the pain and possible reasons.
- Magnetic resonance imaging (MRI) or computed tomography (CT) scan can detect multiple sclerosis or tumors.
- Magnetic resonance angiography (MRA) may detect if a blood vessel is putting pressure on the trigeminal nerve.
Treatment with Drugs
Treatment of trigeminal neuralgia mainly involves the use of certain medicines. Other options such as surgery are considered when the medicines either become ineffective or start producing side effects. However, even surgical intervention in long term cases does not preclude the use of medicines for a prolonged period thereafter.
Trigeminal neuralgia may resolve spontaneously after a few months and remain in a state of remission for a period of time. However, it tends to recur more frequently and intensely in the future and medication may offer limited effectiveness in the long term.
Oral Drugs
Drugs aim to reduce or block the pain signals sent to the brain. Anticonvulsants like carbamazepine, oxcarbazepine, lamotrigine, phenytoin, and gabapentin are commonly prescribed for trigeminal neuralgia. Though these drugs are effective, they may cause side effects like dizziness, drowsiness, confusion, nausea, and double vision.
- Carbamazepine is the most effective anti-convulsant but in some people, it can trigger a serious drug reaction.
- Antispasmodic medicines or muscle relaxants (like baclofen) may be used alone or in combination with phenytoin or carbamazepine.
- Tricyclic antidepressants (like amitriptyline, nortriptyline) may be recommended for treating depression in patients with trigeminal neuralgia.
Injections
- Alcohol injections can numb the affected areas of the face and bring temporary pain relief. This method may have side effects like bleeding and infections at the injection site, and damage to nearby nerves.
- Glycerol injections damage the trigeminal nerve and blocks pain signals. Side effects of these injections may include facial numbness or tingling.
Trigeminal Neuralgia Surgery
Surgery aims at removing or easing the pressure or mechanical irritation of the nerve.
- Gamma-knife radiosurgery (GKR) delivers radiation to the root of the trigeminal nerve. The procedure is more effective and safe when compared with other surgical options.
- In microvascular decompression (MVD) surgery, the blood vessels that are in contact with the trigeminal root are relocated or removed. This removes the pressure on trigeminal nerve. In rare cases, MVD may result in loss of hearing, double vision, facial weakness or numbness, stroke or death.
- Balloon compression involves inserting a balloon with the help of a needle through the face and into the base of the skull. Once the balloon is inflated, the resulting pressure damages the nerve and blocks pain signals.
- Trigeminal rhizotomy involves cutting part of the trigeminal nerve at the base of the brain. This blocks the pain but the face will be numb permanently.
- In radiofrequency thermal rhizotomy, an electric current destroys nerve fibers associated with pain. The procedure results in some facial numbness.
References :
http://emedicine.medscape.com/article/1145144-overview
http://www.ninds.nih.gov/disorders/trigeminal_neuralgia/detail_trigeminal_neuralgia.htm