Sleeping Sickness (African Trypanosomiasis)
What is sleeping sickness?
Sleeping sickness, also called African trypanosomiasis, is a caused by a small parasite Trypanosoma brucei. It is confined to sub-Saharan Africa. Although the term sleeping sickness may be associated with other infections which causes similar symptoms, the term is more commonly associated with African trypanosomiasis.The infection is transmitted by the bite of an infected tsetse fly. The condition is fatal if prompt medical treatment is not implemented as it progresses to the second phase where the brain and nerves are affected.
Types of African Trypanosomiasis
There are two similar-looking sub-species of Trypanosoma brucei protozoan: T. brucei rhodesiense and T. brucei gambiense.
- T. brucei rhodesiense causes East (or Rhodesian) African trypanosomiasis.
- T. brucei gambiense causes West (or Gambian) African trypanosomiasis.
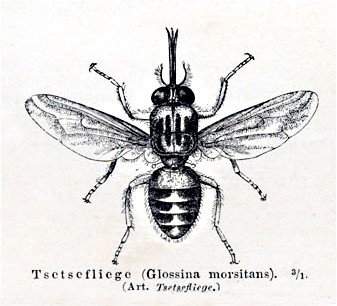
Infected tsetse flies (Glossina) bite humans and thus transmit these parasites. G. palpalis flies spread West African trypanosomiasis by transmitting T. brucei gambiense whereas G. morsitans spread East African trypanosomiasis by transmitting T. brucei rhodesiense.
Humans are the only reservoirs of infection in West African trypanosomiasis. East African trypanosomiasis, however, has animal vectors too and hence is called a ‘zoonotic’ infection.
Picture of the tsetse fly from Wikimedia Commons
Who gets sleeping sickness?
Travelers get African trypanosomiasis by visiting endemic areas in Africa. It affects about one US traveler every year. In majority of the cases, the infections acquired in East African game parks and are caused by T. brucei rhodesiense. Sleeping sickness is very common in some countries of East and West Africa and threatens millions of natives and travelers. It can affect people of all ages, races and genders.
What does sleeping sickness do?
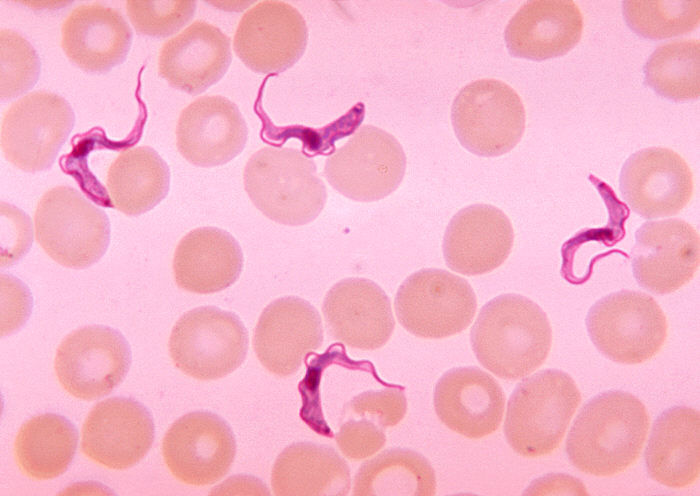
Humans acquire T. brucei infection through tsetse fly bite. The bite may cause a painless skin sore at the site, which may disappear on its own in some weeks. The introduced trypomastigotes mature and grow in the blood and lymph glands. The infection causes discomfort, fever, skin rash, and muscle wasting. If the parasites reach the brain, they may cause mental and behavioral changes (like encephalitis, coma). Death may occur.
Picture of trypanosome parasite in the blood from Wikimedia Commons
The human immune system tries to fight off this infection but the parasites can escape these defense mechanisms by changing their forms. After evading the immune responses, the parasites grow rapidly in blood and lymph nodes and reach organs like the brain and the heart. On the other hand, the immune system’s continued response at these sites, results in the breakdown of red blood cells, thereby leading to anemia, and inflammation of heart and brain and its meninges.
Due to body’s hypersensitive reaction to the parasites, many skin problems occur. Itching, swelling, and hives are commonly seen. The gastrointestinal system (GI) and liver are also affected.
Symptoms and Stages
The symptoms of sleeping sickness vary in different phases and can be grouped as early and late.
Stage 1 – Early Stage
This is known as the hemolymphatic stage.
- Appearance of painless skin sores 5-15 days after the bite.
- Intermittent fever, discomfort, muscle pain, joint pain and headache (3 weeks after bite).
- Swollen lymph nodes.
- Enlarged spleen.
- Fast heartbeat.
- Swelling on the face.
- Appearance of itchy welts of rashes 6 to 8 weeks after onset.
- Appearance of macules on body.
Stage 2 – Late Stage
This is known as the neurological stage.
- Persistent headaches that do not respond to pain-relievers.
- Daytime sleepiness and nighttime sleeplessness.
- Mood swings and depression.
- Loss of appetite.
- Weight loss.
- Muscle wasting.
- Seizures in children.
- Coma.
- Shaking.
- Difficulty walking.
East African trypanosomiasis develops within a month after being bitten, whereas West African trypanosomiasis begins months to a year after contracting the infection. Untreated trypanosomiasis is fatal. If not treated, East African trypanosomiasis can result in death within few weeks or months.
Causes of Sleeping Sickness
Both forms of African trypanosomiasis, East African and West African, are caused by bites from infected tsetse flies. Trypanosomes are protozoan parasites that complete their life cycle in two hosts – mammals and arthropods. If a human reservoir (in West African trypanosomiasis) or an animal reservoir (in East African form) is bitten by a tsetse fly, the trypanosomes are ingested with the blood.
Picture of the life cycle of the sleeping sickness parasite sourced from CDC.gov
At this point the life cycle of the parasites starts. The trypanosomes multiply for 2 to 3 weeks in the mid-gut of tsetse fly. After that, they migrate to the salivary gland, where they grow into the infective form, called epimastigotes. These trypomastigotes infect humans who are then bitten by the tsetse fly.
The main risk factors is travelling to parts of Eastern, Western and Central Africa.
African Trypanosomiasis Diagnosis
The presence of any of the signs and symptoms, particularly in a patient with a recent history of traveling to endemic areas, should warrant the need for further investigation. The following tests can be performed to diagnose sleeping sickness:
- Lab tests:
– Blood samples are tested for complete blood count, hemoglobin levels, and presence of trypanosomes in the body. Anemia, high immunoglobulin M (IgM) level, low platelet count, and low albumin levels are commonly seen in patients.
– In the early stages of infection when the number of circulating parasites is highest, lymph node aspiration or wet blood smear can detect mobile trypanosomes.
– Cerebrospinal fluid (CSF) can be collected through a lumbar puncture from patients complaining of mental and behavioral changes. CSF may also be checked for trypanosomes.
- Imaging studies: A computed tomography (CT) scan or a magnetic resonance imaging (MRI) scan can detect swelling of brain, indicating a late-stage infection.
- Antibody detection: A fast and highly sensitive test called card agglutination test for trypanosomiasis (CATT) can be used to diagnose West African trypanosomiasis. This test can be performed on blood sample, CSF, bone marrow aspirate, or tissues.
Treatment for Sleeping Sickness
The treatment aims at:
- Removing the parasitic infection from the body
- Managing fever, body pain, and discomfort
- Preventing mental or behavioral changes often associated with complications
Medications
Anthelmintics are given to treat parasitic infections. Small doses of these drugs are sufficient to clear the parasitic infection.
- Suramin inhibits growth of parasites. It is less toxic and more effective than pentamidine which is used for early stage sleeping sickness. It cannot cross the blood-brain barrier though.
- Pentamidine isethionate is used for early (or stage 1) African trypanosomiasis. It is given intravenously. Like suramin, pentamidine isethionate too cannot cross the blood-brain barrier.
- Melarsoprol kills the trypanosomes. It is very effective in treating late stage of infection. It can be toxic and even fatal in 5% of cases.
- Eflornithine treats late (or CNS) disease in patients with West African trypanosomiasis. It is less toxic and is well tolerated compared to arsenic drugs.
Treating stage 1 (hemolymphatic stage) sleeping sickness
- Suramin is given for East African trypanosomiasis caused by T. brucei rhodesiense.
- Pentamidine isethionate or suramin are given for West African trypanosomiasis caused by T. brucei gambiense.
Treating stage 2 (neurologic/CNS stage) sleeping sickness
- Melarsoprol or eflornithine are given for West African trypanosomiasis caused by T. brucei gambiense.
- A combination of melarsoprol and nifurtimox works best against T. brucei gambiense trypanosomiasis.
References :
http://www.cdc.gov/parasites/sleepingsickness/disease.html