Pseudomembranous Colitis (Clostridium difficile Infection)
What is Pseudomembranous Colitis?
Pseudomembranous colitis is a condition where there is inflammation of the colon due to an overgrowth of certain species of bacteria known as Clostridium difficile. In some rare cases it may be arise with the overgrowth of other microorganisms. Pseudomembranous colitis is also known as antibiotic-associated colitis or antibiotic-associated diarrhea because the predominant symptom is diarrhea and tends to arise after the use of antibiotics. However, it is possible for the condition to arise in patients who have not recently used antibiotics. Pseudomembranous colitis is a potentially life-threatening condition but can be effectively treated and managed in most cases.
How Common is Pseudomembranous Colitis?
Pseudomembranous colitis is one of the most common nosocomial infections, meaning infections that originate while in hospital. It occurs in about 0.5% of all patients admitted to hospitals in the United States. Older patients, over the age of 65 years, are at a significantly greater risk. Although the condition is potentially life threatening, death occurs in less than 2% of patients who develop pseudomembranous colitis.
What Happens in Pseudomembranous Colitis?
Clostridium difficile is a spore forming bacteria that is most often acquired when in hospital. In most cases it does not pose a significant health risk as not all Clostridium difficile strains are pathogenic and the normal intestinal flora (“good bowel bacteria”) prevents an overgrowth. However, with the use of antibiotics, weakened immunity and particularly with hospitalization, these bacteria may get the opportunity to thrive relatively unchecked in the human colon. This is more likely to occur with oral administration (by mouth) of antibiotics.
Picture of C.difficile bacteria from Wikimedia Commons
Toxins
The bacteria that are pathogenic, more correctly referred to as toxigenic Clostridium difficile, secretes toxins which causes bowel inflammation. Most toxigenic C.difficile secrete two such toxins – toxin A and toxin B – with a small number of these bacteria secreting an additional toxin known as binary toxin. Some of these toxins like toxin A specifically injures cells lining the gastrointestinal tract. With injury, inflammation within the colon ensures. Therefore the term ‘colitis’.
False Membrane
The bowel wall becomes swollen (edematous) and the junctions between the mucosal cells is disrupted. Fluid is able to secrete out into the bowel lumen thereby contributing to watery diarrhea in pseudomembranous colitis. Some cells die. Continuation of the inflammatory process eventually reaches a point where there is a discharge from the bowel wall that looks like a membrane. It is responsible for the term pseudomembranous colitis. This pseudomembrane (meaning ‘false membrane’) is composed of mucus with connective tissue like fibrin and inflammatory cells as well as remnants of the bacteria and mucosal cells.
Signs and Symptoms
The symptoms of pseudomembranous colitis can begin as early as 1 to 2 days after starting antibiotics or as late as 5 to 10 days thereafter.It is important to remember that antibiotics may not necessarily precede the onset of pseudomembranous colitis. Some patients can also develop the condition a week or more after discontinuing treatment. In rare cases, pseudomembranous colitis can develop up to 2 months after using antibiotics.
Diarrhea
Pseudomembranous colitis diarrhea can range from mild to severe. In milder cases a person may have between 3 to 6 stools a day compared to 20 stools or more per day in severe cases.
- The stools are typically watery and there is a high risk of dehydration.
- Milder cases may present with loose but not watery stool.
- Bloody stools are more likely to be seen in more severe cases.
- Pus and/or mucus in the stool may also be present.
Abdominal pain
Pain in the abdomen is a common symptom. Most patients complain of cramping. Severe cases may present with intense pain throughout the abdomen. The pain may be constant or episodic, aggravated before stool, during bowel movement and possibly ease after passing stool. The urge to pass stool is usually constant and sometimes confused with the abdominal pain. Very severe pain of sudden onset (acute abdomen) can be a sign of complications such as toxic megacolon or rupture of the colon.
Other symptoms
- Fever
- Nausea
- Vomiting (rare)
- Loss of appetite
- Fatigue
- Malaise
- Constipation (rare)
The signs and symptoms of dehydration may also be present.
Causes of Pseudomembranous Colitis
Pseudomembranous colitis is a result of Clostridium difficile overgrowth in the colon following antibiotic use. However, this is not necessarily the cause in every case. Although the terms antibiotic-associated colitis, antibiotic associated diarrhea, Clostridium difficile colitis and C. difficile infection is used interchangeably with pseudomembranous colitis, this can be misleading because:
- Not every case of pseudomembranous colitis is due to Clostridium difficile infection.
- Not every case of pseudomembranous colitis is associated with antibiotic use.
However, the majority of cases arises with Clostridium difficile infection following the use of antibiotics.
Antibiotics
Although any antibiotic may increase the chance of developing pseudomembranous colitis, the more commonly implicated antibiotics include :
- Clindamycin
- Cephalosporins such as cefixime and cefpodoxime
- Penicillins such as amoxicillin and ampicillin
- Quinolones such as ciprofloxacin and levofloxacin
Bacteria
Clostridium difficile is the main cause of pseudomembranous colitis. Other bacteria that may be involved, although very rare, includes :
- Staphylococcus species
- Certain strains of Clostridium perfringens
- Campylobacter species
- Listeria species
- Salmonella species
Risk Factors
Apart from people who have used antibiotics being at risk of developing pseudomembranous colitis, other risk factors may include :
- Elderly people, over 65 years.
- Hospitalized patients.
- Having recently undergone intestinal surgery.
- Nursing home residents.
- Immunocompromised patients.
- Cancer patients undergoing chemotherapy.
- Patients with pre-existing colon diseases.
- Parenteral nutrition (feeding through an IV drip).
Diagnosis of Pseudomembranous Colitis
The signs and symptoms are not specific for pseudomembranous colitis. However, greater awareness about the risk of this condition in hospitalized patients and those undergoing antibiotic treatment often raises the suspicion about the condition. The diagnosis may also be confirmed if the condition resolves with discontinuing antibiotics and commencing probiotics. Antibiotics should not be discontinued without medical supervision. Specific investigations are more effective in confirming the diagnosis. These tests and scans include :
- Stool culture – grows the bacteria in a laboratory.
- Stool immunoassay – confirms the presence of C.difficile toxin in the stool.
- Colonoscopy – verify the typical pseudomembrane appearance of the colon.
- X-ray or computed tomography (CT) scan – detect complications like rupture of the colon or toxic megacolon.
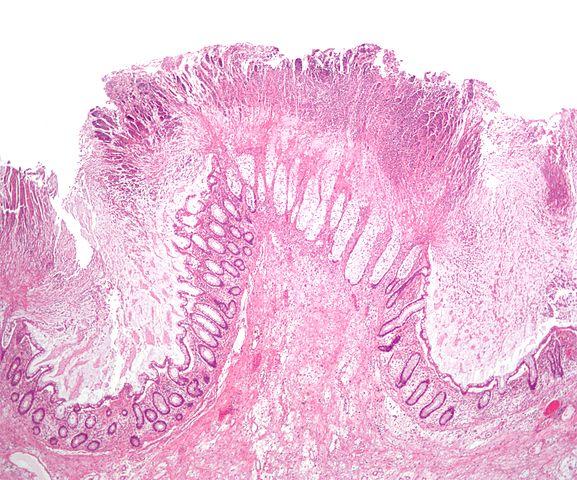
Picture of pseudomembrane in the colon from Wikimedia Commons
Treatment of Pseudomembranous Colitis
Discontinuing the offending antibiotic is the first step in treating and managing pseudomembranous colitis. The condition may resolve on its own within 2 to 3 days thereafter. If antibiotics are still necessary, the type of antibiotic may be changed to an alternative that is less likely to contribute to pseudomembranous colitis. More specific measures for treating pseudomembranous colitis includes :
- Antibiotics to eradicate the Clostridium difficile overgrowth. Vancomycin and metronidazole may be used although even these antibiotics can sometimes contribute to pseudomembranous colitis.
- Surgery involving removal of part of the colon (partial colectomy) is rarely conducted but may be a consideration in severe pseudomembranous colitis. It is more likely to be conducted in cases where the condition is severe and not responding to medication or there are complications like toxic megacolon, colon rupture or peritonitis.
Oral rehydration solutions (ORS) should be used to prevent dehydration. In severe cases, intravenous (IV) fluid and electrolyte replacement is necessary.
How to Prevent Pseudomembranous Colitis
Due to greater awareness about pseudomembranous colitis, specific measures can be taken to prevent the condition. These measures are usually effective in most patients using antibiotics. Probiotics containing Saccharomyces boulardii with or without Lactobacillus casei may be used with antibiotics or immediately after completing a course of antibiotics to prevent pseudomembranous colitis. These probiotics are also useful in the treatment of the condition once it arises. Some patients may develop secondary lactose intolerance so using live culture yogurt may not be advisable as it can exacerbate the diarrhea.
References
www.mayoclinic.org/diseases-conditions/pseudomembranous-colitis/