Low Blood Sugar (Glucose) Hypoglycemia Symptoms, Causes, Treatment
What is hypoglycemia?
The term low blood sugar is commonly used to refer to a drop in blood glucose levels below 54mg/dL or 3mmol/L. This state is referred to as hypoglycemia. In a person with diabetes, a blood glucose level below 63mg/dL or 3.5mmol/L is referred to as hypoglycemia.
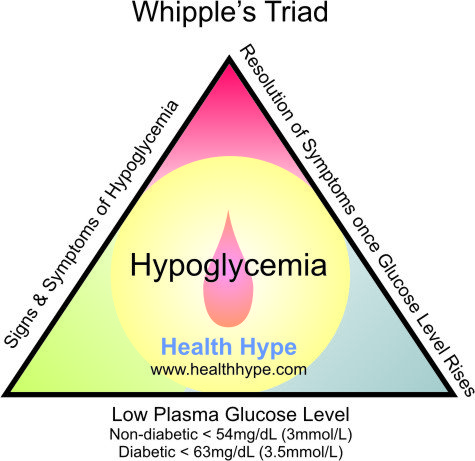
Medically, hypoglycemia may be diagnosed by three factors which is known as Whipple’s triad :
- Signs and symptoms of hypoglycemia
- Low plasma glucose level (as mentioned above)
- Resolution of hypoglycemia signs and symptoms once the plasma glucose (blood sugar) level rises
Whipple’s Triad
Blood Sugar Range (Levels)
The term low blood sugar is often used frivolously to describe a range of symptoms that may or may not be related to a low plasma glucose concentration. There is also confusion relating to the blood glucose levels that can be classified as hypoglycemia.
In some patients, the symptoms of hypoglycemia may be evident at a blood glucose level below 70mg/dL (3.8 mmol/L). This is more frequently seen in diabetics. In others, the signs and symptoms may only be evident as the blood glucose levels drop below 60mg/dL (3.3mmol/L). The blood glucose levels of newborn babies (neonates) may drop as low as 30 mg/dL (1.7 mmol/L) in the first day of life and should be attended to immediately with feeding.
Non-Diabetics
- Pre-Prandial– Fasting, Before Meals, Upon Waking
- In a person without diabetes, the normal fasting glucose levels may be between 70mg/dL (3.9 mmol/L) and 99mg/dL (5.5mmol/L).
- Post-Prandial– After Eating (1 to 2 hours)
- After eating, the blood glucose level can rise to, but should not exceed, 140mg/dL (7.8mmol/L).
- Blood glucose levels below 54mg/dL (3mmol/L) is considered as a low blood sugar level and is diagnosed as hypoglycemia if it meets with the guidelines as per Whipple’s triad.
Diabetes and Pre-Diabetes
- Pre-Prandial– Fasting, Before Meals, Upon Waking
- In diabetics, the fasting blood glucose level may range from 70mg/dL (3.9mmol/L) to 140mg/dL (7.8mmol/L).
- In pre-diabetes (impaired glucose tolerance), the fasting level is usually below 125mg/dL (6.9mmol/L).
- Post-Prandial– After Eating (1 to 2 hours)
- After eating, the blood glucose levels in a diabetic may exceed 200mg/dL (11.1mmol/L). This is not ideal and better management should aim to limit the rise in blood glucose levels of diabetics after eating to 180mg/dL (10mmol/L) or less.
- With pre-diabetes (impaired glucose tolerance), the blood glucose levels after eating is usually less than 200mg/dL (10mmol/L). If it exceeds this level, it is a good indication that the person is a diabetic.
Refer to Blood Sugar Levels for Diabetes and Impaired Glucose Tolerance (high readings) for more information.
Symptoms of Hypoglycemia
The signs and symptoms of hypoglycemia can be divided into two categories :
- Autonomic
- Neuroglycopenic
There are are also general and non-specific signs and symptoms which should not be used in isolation to diagnose hypoglycemia. These general symptoms include nausea, fatigue, and headaches. Often the term ‘low blood sugar’ is used frivolously to explain the cause of these symptoms although other causes could account for it.
Autonomic
When the blood glucose levels drop significantly, the body releases epinephrine. This triggers certain processes like releasing the glucose stored in the liver (glycogen) in an attempt to stabilize the blood glucose levels. Epinephrine also affects the nervous system and results in these characteristic signs and symptoms :
- Anxiety
- Dizziness
- Hunger
- Palpitations
- Sweating
- Trembling
These symptoms are the early warning signs but may be absent in certain cases. In patients who experience frequent episodes of hypoglycemia, the body may stop releasing epinephrine. This is known as hypoglycemic-associated autonomic failure (HAAF) or is also referred to as hypoglycemia unawareness. The blood glucose levels continue to drop until the neuroglycopenic symptoms may be evident. It may only be at this point that the appropriate measures are implemented.
Neuroglycopenic
As the blood glucose levels continue to drop without any intervention, the glucose supply to the brain is severely impaired and may result in the symptoms listed below.
- Blurred vision
- Confusion
- Difficulty concentrating
- Drowsiness
- Irritability, anger
- Poor coordination
- Speech difficulty
Eventually seizures and even a coma may ensue. Changes in behavior at this stage may resemble inebriation (alcohol intoxication, drunkenness) and is sometimes mistaken for alcohol dementia in alcoholics.
Causes of Hypoglycemia
The body maintains the blood sugar levels within a narrow range between 72 mg/dL (4mmol/L) and 104mg/dL (5.8mmol/L). It is not abnormal for these levels to sometimes rise above 108mg/dL (6mmol/L) or drop as low as 63mg/dL (3.5mmol/L).
Hypoglycemia can be defined according to the presence of the features known as Whipple’s triad. This is often seen in a blood glucose level below 54mg/dL (3mmol/L) in a person who is not diabetic and blood sugar levels below 63mg/dL (3.5mmol/L) in diabetics.
Meals, Fasting and Dieting
- Eating small amounts of food, missing meals or eating infrequently and waiting for long periods between meals may all cause low blood sugar levels.
- Strict dieting or fasting often result in severe hypoglycemia. The signs and symptoms of hypoglycemia is not related to any “detoxification” process as claimed by some weight loss and detoxification programs. If left untreated, it can result in serious and even life-threatening complications. Dehydration may also play a part in these cases of hypoglycemia.
Physical Activity and Exercise
- Strenuous physical activity which is not customary for a person can cause a significant drop in the blood sugar levels, especially if there is inadequate food intake during this period.
- Exercise which is not a usual practice or unexpectedly excessive may also cause low blood sugar levels.
- In a person who is accustomed to excessive physical activity and strenuous exercise, the blood sugar levels may not drop to low levels as quickly as in an unfit person. The use of sports drinks may also help to prevent hypoglycemia.
Alcohol
- Alcohol consumption can increase insulin levels which causes a drop in the blood glucose levels.
- Diabetics using insulin and other medication that increase insulin production may find that the effect is exacerbated leading to dangerously low blood sugar levels.
- Consuming small meals before and during alcohol intake can reduce this effect. Binge drinking should be avoided.
Diabetes
Hypoglycemia in diabetics may occur as a result of :
- Excessive and improper use of insulin and other anti-diabetic agents.
- Increased subcutaneous fat deposits (lipohypertrophy) at injection sites for insulin administration may affect insulin absorption.
- Alcohol consumption (mentioned above) and drug interactions with other medicines that may affect insulin levels.
- Breastfeeding by diabetic mothers.
Diabetic patients should be aware of nocturnal hyperinsulinemia as blood glucose levels drop during sleep and incorrect administration of insulin at night could result in hypoglycemia.
Age
- Hypoglycemia is more likely to occur in infants and the elderly due to poor glucose tolerance.
- Age is a risk factor rather than a cause of hypoglycemia.
Other Disorders
- Malabsorption syndromes may affect the absorption of glucose and other nutrients thereby resulting in low blood sugar levels.
- Conditions that affect normal peristaltic activity like gastroparesis.
- Hypoglycemia may be a consequence of other disorders like :
- Addison’s disease
- Cushing’s syndrome*
- Pancreatic cancer or other tumors of the pancreas – insulinoma is a tumor of the pancreatic islet cells that secretes insulin.
- Pituitary insufficiency
- Liver failure
- Causes of delayed gastric emptying (gastroparesis, gastric outlet obstruction)
* Cushing’s syndrome usually results in hyperglycemia but acute hypoglycemia attacks may be occur.
Treatment of Hypoglycemia
Mild hypoglycemia is not necessarily a medical emergency unless the excessive use (overdose) of anti-diabetic agents or insulin has been implicated as a possible cause. This could rapidly progress into severe hypoglycemia. In most instances it can be managed in the home environment with readily available food ingredients.
Even if medical attention is not required immediately in a case of mild hypoglycemia, the cause should be investigated and identified to prevent further episodes. However, in cases of severe hypoglycemia, these measures are only useful temporarily and immediate medical attention is necessary.
Severe hypoglycemia is more likely to occur in diabetics – particularly insulin-dependent diabetes. The regular use of a blood glucose monitoring device is therefore essential and diabetics should not rely solely on their perception of low blood sugar levels.
If left untreated, hypoglycemia can lead to death. This is not only a concern for older patients with diabetes. Sudden death due to hypoglycemia may occur in a young person with type 1 diabetes. This is not common but typically occurs during sleep possibly as a result of cardiac arrhythmias induced by hypoglycemia.
Treatment of Mild Hypoglycemia
The early warning signs as outlined in the Hypoglycemia Signs and Symptoms should be present and a blood glucose level below 70mg/dL (3.8mmol/L) in diabetics or 63 mg/dL (3.5 mmol/L) in non-diabetics is sufficient to warrant the implementation of the measures below.
- A fast-acting (simple) carbohydrate like glucose needs to be administered orally.
- 15 grams may be given in the form of a glucose solution, tablets, gel.
- A confectionery (sweet) may be helpful if no other measures are available. Table sugar, fruit juice and sodas may also be used.
- A snack containing long-acting starch (complex carbohydrate) should follow – example toast.
- Snacks should be avoided if hypoglycemia is suspected as a result of overdose, especially intentional, and immediate medical attention should be sought. Glucose can be administered orally in these instances.
It is acceptable to implement these measures without a blood glucose level assessment if a home monitor is unavailable. If a home glucose monitor is available, the blood glucose levels should be assessed every 15 minutes until the glucose levels return to an acceptable range and the signs and symptoms abate.
A repeat dose of 15 grams of glucose may be necessary. Other signs and symptoms (neuroglycopenic) like confusion, inability to concentrate and poor coordination may take up to 60 minutes to resolve. If the blood glucose levels continue to drop despite the administration of glucose, this should be considered as severe hypoglycemia.
Emergency Treatment of Severe Hypoglycemia
Severe hypoglycemia is not solely dependent on the blood glucose levels as some patients are cautious about seeking emergency medical attention despite the presence of serious signs and symptoms. Difficulty speaking, drowsiness, impaired coordination and mental confusion is sufficient to determine a case of severe hypoglycemia, especially if a patient is unresponsive to glucose, and should be differentiated from alcohol or drug intoxication.
Seizures, blackouts or a coma is a clear indication of severe hypoglycemia unless it is caused by other disorders. Ideally severe hypoglycemia should not be managed in the home environment but immediate measures are necessary until medical attention can be secured.
- Conscious patients who are able to swallow :
- 25 grams of glucose in solution, tablet or sweet form.
- Glucose gel or even honey can be rubbed on the inner lining of the mouth (cheek).
- Semiconscious or unconscious patients :
- These measures need to be conducted by a trained medical professional.
- Intravenous (IV) – 75ml of 20% dextrose or 25 to 50ml of 50% dextrose.
- Intramuscular (IM) – 1mg glucagon if no IV access.