Liver Cirrhosis Causes, Early and Late Signs and Symptoms
The liver is a versatile organ that metabolizes nutrients, wastes, toxins, drugs and other substances. It has various secondary roles including acting as a reservoir for blood. The liver has a complex architecture involving lobules containing hepatocytes (liver cells) and weighs about 1.6 kg (2.5% of the average adult body weight). Blood is received via the portal vein and hepatic artery, the former which brings blood to the liver to be processed and the latter nourishes the liver tissue with oxygen and nutrients. Waste products that are not passed out into the blood to be eventually be filtered by the kidneys make up bile which is then dumped in the gut during digestion and expelled in the fecal matter.
What is liver cirrhosis?
Cirrhosis of the liver (hepatic cirrhosis) is fibrosis of the liver tissue with abnormal nodule formation that structurally deforms the liver. It is the end stage of chronic liver disease and a common cause of death worldwide. In countries like the United States, liver cirrhosis is among the top 15 causes of death and the most common cause of liver-related death. Contrary to popular belief, liver cirrhosis does not only occur as a consequence of alcohol abuse and there are many other liver and systemic diseases that may result in cirrhosis.
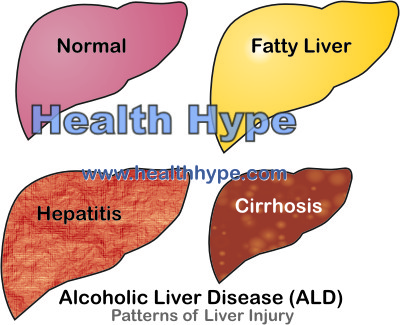
While mild cases may be reversible, most cirrhosis cases are advanced and the damage therefore irreversible. It is helpful to understand the patterns of liver disease which includes inflammation (hepatitis), fat deposition (fatty liver) and cirrhosis. Below is a look at alcoholic liver disease (ALD) specifically but these changes can be seen with any liver disease.
Liver cirrhosis develops slowly over years although with severe liver injury it can develop within weeks. It is achieved by activation of hepatic stellate cells which is then transformed into collagen-producing cells that also manufactures chemical mediators of inflammation. Prolonged inflammation of the liver eventually leads to death of hepatocytes. Fibrous septa form by the process of fibrosis mediated by the stellate cells. Eventually these is multiple nodules in the liver, both small (less than 1mm in diameter) and large (various sizes). This contributes to the two types of cirrhosis – micronodular cirrhosis and macronodular cirrhosis.
Causes of Cirrhosis
The two most common causes of cirrhosis includes alcohol consumption (alcoholic liver disease), and chronic viral hepatitis.
Alcoholic Liver Disease
This arises with long term and heavy drinking and is therefore more frequently seen in alcoholism. The metabolites of high quantities of alcohol are toxic to the liver cells and causes diffuse injury. Fat deposition (fatty liver disease) initially occurs with several episodes of acute inflammation (hepatitis) and eventually this progresses to cirrhosis. ALD may also arise due to an interplay of heavy alcohol consumption with other factors like malnutrition, autoimmune factors and genetic factors. Read more on alcoholic liver disease.
Viral Hepatitis
Viral hepatitis is liver infection caused by one of the five known hepatitis viruses. The most common of these hepatitis virus to lead to a chronic infection is hepatitis B and hepatitis C. Both these types of hepatitis viruses can be transmitted through blood, saliva and semen and is therefore more common with IV drug users, health care workers and sex workers. The condition is further compounded when there is underlying alcoholic liver disease. Read more on the types of hepatitis.
Non-Alcoholic Fatty Liver Disease
This type of liver disease is seen with little or no alcohol consumption. Fat deposition occurs similar to alcoholic liver disease and this can progress further more serious liver injury and cirrhosis. The exact cause is unclear but it is believed to be a result of difficulty on the part of the liver to break down fats.
Other Causes
These causes constitute a minority of cirrhosis cases. It includes a wide range of disorders including :
- Autoimmune hepatitis
- Primary sclerosing cholangitis
- Primary and secondary biliary cirrhosis
- Cystic fibrosis
- Hemochromatosis
- Wilson’s disease
- Alpha 1-antitrypsin deficiency
- Chronic venous outflow obstruction
- Unknown causes
Signs and Symptoms
Almost half of patients with liver cirrhosis are asymptomatic meaning there is no obvious symptoms.
Early Symptoms
In the early stages the symptoms may be non-specific and may include :
- Weight loss
- Lack of appetite
- Weakness
- Fatigue
- Nausea and vomiting
- Muscle cramps
- Abdominal discomfort
Late Symptoms
Although many of these late signs may first be detectable in the latter part of the early stages, it becomes more prominent later in the disease progression. These signs and symptoms, when seen together, should be considered more specific for cirrhosis.
- Enlarged liver (hepatomegaly) is more prominent in alcoholic liver disease and hemochromatosis.
- Shrunken liver occurs gradually and is more common in other causes particularly with viral hepatitis and autoimmune hepatitis.
- Abdominal distension usually associated with ascites (fluid accumulation in the abdominal cavity).
- Jaundice which is a yellow discoloration of the skin and sclera (eyes).
- Enlarged spleen (splenomegaly)
- Bleeding which is evident as bruises, purplish spots due to bleeding (purpura) and in severe cases even vomiting of blood (hematemesis).
- Hepatic encephalopathy which is an alteration of the mental state that may vary from confusion to even coma.
Other clinical features which may or may not be present and can vary in severity in intensity includes :
- Palmar erythema – redness of the palms.
- Digital clubbing – abnormal rounding of the fingers.
- Pigmentation – abnormal skin discoloration.
- Spider telangiectasia – enlarged small blood vessels commonly referred to as spider veins.
- Cyanosis – bluish discoloration of the skin due to low oxygen levels.
- Dupuytren’s contracture – hand deformity.
- Hair loss
- Diminished libido
- Changes in breast size, typically reduction in size in women and possible enlargement in men.
- Changes in sexual function and reproductive health in both genders.