Dysphagia (Difficulty Swallowing), Types, Symptoms, Diagnosis
What is Dysphagia?
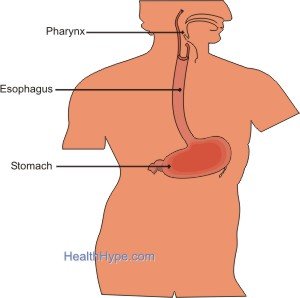
Dysphagia is the medical term for any difficulty with swallowing. In this instance difficulty not only means that the ability to move food and drinks from the throat into the stomach is hampered but there could also be pain when swallowing. Sometimes, the ability to swallow is completely impaired. Swallowing pushes food from the back of the mouth, into the throat and down the esophagus (food pipe).
It does not enter the lungs because of a flap called the epiglottis, which closes entry into the airway. The muscles of the esophagus then takes over to push the food down towards the stomach, where the lower esophageal sphincter opens and lets food into the stomach.
There are two types of dysphagia – oropharyngeal (mouth-throat) and esophageal (food pipe). Although swallowing is only thought of as the process of food exiting the mouth and throat, it does involve the transport all the way into the stomach. This entire process is carried out by the muscles of the tongue, throat and esophagus and coordinated by the impulses sent from the brain through nerves.
Dysphagia should not be confused with the feeling of a lump in the throat, when no mass exists, as this is known as globus sensation.
Symptoms and Types
There are two types of dysphagia – oropharyngeal and esophageal. This has been discussed further under the causes of dysphagia.
The first part of swallowing involving the mouth and throat (pharynx) is a reflex action which quickly moves food and liquid into the esophagus. Failure to either move the food into the esophagus or pass it out into the front of the mouth at this stage will lead to gagging, drooling, coughing or regurgitating of food through the nose. This is known as oropharyngeal dysphagia. There may also be the sensation of food being stuck in the throat or back of the mouth.
The second part of swallowing involving the food pipe (esophagus) is under the control of network of nerves in the area known as the myenteric plexus and the brainstem. A ‘wave’ created by the sequential contraction of muscles of the esophagus transports the food down to the stomach. This is known as peristalsis. Any impairment of the movement of food down the esophagus and into the stomach is known as esophageal dysphagia. One of the symptoms characteristic of this type of dysphagia is a discomfort or pain in the chest (breastbone pain) which is often described as a tightness or pressure. This is sometimes described as the sensation that ‘something is stuck in the chest’.
Other signs and symptoms of dysphagia may include :
- A lack of appetite and loss of weight are common signs of dysphagia and should not be mistaken for one of the different types of eating disorders.
- Heartburn.
- Sore throat.
- Pain upon swallowing (odynophagia).
- Excessive belching.
- Chest pain (refer to Gastric Chest Pain).
- Regurgitating food and drink.
- Recurrent pneumonia – a complication of tracheal aspiration.
- Prolonged feeding times.
- Unusual eating habits and behavior which are common in children and infants who cannot express that they are experiencing difficulty with swallowing.
If there is a total inability to swallow, possibly indicating a complete obstruction, weight loss or the development of any neurological signs and symptoms not previously assessed by a doctor, then emergency medical treatment is essential.

Diagnosis of Dysphagia
Dysphagia, or difficulty swallowing, is any disruption with the process of swallowing or the swallowing reflex. It may either be a partial or total impairment of the swallowing process although the latter is less frequently seen. There are two types of dysphagia which may be due to a number of factors as discussed under the causes of oropharyngeal dysphagia and esophageal dysphagia. Assessing the cause of dysphagia involves both a physical examination by a doctor as well as additional diagnostic investigations that may be deemed necessary following this examination.
Examination and Tests
Visual Examination
Examination of the oral cavity and pharynx is essential to assess any oropharyngeal causes of dysphagia. Dental problems, inflammation of the lining of the mouth and throat, sores, plaques and masses need to be identified. Anatomical abnormalities, like those of the the soft palate, should also be noted.
Speech Problems
Problems with speech, either the production of sound (dysphonia), which may be evident as hoarseness or a whispering tone of the voice, or articulation (dysarthria), which may be evident as slurred speech, will also assist with identifying possible causes. Dysphonia or dysarthria may be indicative of neurological or muscular disorders which could also affecting the swallowing mechanism.
Neurological Test
Testing of cranial nerves V (trigeminal), VII (facial), IX (glossopharyngeal), X (vagus) and XII (hypoglossal) is necessary to identify neurological causes of dysphagia.
- Trigeminal Nerve (CN V)
- The main nerve responsible for controlling the muscles of the mouth for chewing (mastication). Food that is not chewed sufficiently may not pass through the slit created by the palatopharyngeal folds.
- Carries impulses back to the swallowing centers in the brain stem to initiate the swallow reflex.
- Passes impulses from the swallowing center to the muscles of the throat to initiate swallowing.
- Facial Nerve (CN VII)
- Responsible for controlling the lips which helps to push food into the mouth for chewing and keeping the mouth cavity close during swallowing.
- Plays a role in carrying impulses back to the brain stem to initiate the swallow reflex although CN V and CN IX play a larger role in this function.
- Glossopharyngeal Nerve (CN IX)
- Carries impulses from the back of the throat (posterior pharynx) to the swallowing centers in the brain stem.
- Transmits motor impulses from the swallowing center back to the throat muscles to initiate the pharyngeal stage of swallowing.
- Vagus Nerve (CN X) and Hypoglossal Nerve (CN XII)
- Carries impulses from the swallowing center to the throat muscles.
Damage of the swallowing center in the brain stem is seen in diseases like poliomyelitis and encephalitis. Sensory impulses to the swallowing centers may therefore not trigger the swallowing reflex, although the cranial nerves are intact.
Assessment of Reflexes
The gag reflex and cough reflex may both be assessed. This indicates problems with sensory stimulation as well as motor actions as there are common factors between these reflexes and the swallow reflex.
An ’empty’ swallow is necessary to detect the movement of the larynx as described under the swallow reflex. This may indicate problems with the sequence of events that occurs in the pharyngeal stage of swallowing.
Swallowing a small amount of water allows the doctor to observe the process of swallowing. Failure of the act of swallowing to occur (water retained in mouth and larynx does not visibly move as expected), coughing as the glottis fails to close and the water enters the lungs or regurgitating water through the nose as the soft palate fails to close the posterior nares may be observed.

Scans
A range of diagnostic investigation may be necessary depending on the availability of facilities and clinical assessment.
Basic imaging techniques may include :
- Chest and neck x-ray
- Ultrasound
- CT (Computed Topography)
- MRI (Magnetic Resonance Imaging)
These investigations may illustrate :
- Consolidated areas of the lung due to pneumonia may arise as a result of aspiration.
- Structural abnormalities or masses that may be responsible for dysphagia.
Specialist investigations may include :
- Barium swallow and chest X-ray
- Barium swallow and videofluoroscopy (also known as a modified barium swallow, videofluoroscopy swallow study or videoesophagography)
These investigations provide still and dynamic images to assist with identifying any obstructions or dilated gullet (megaesophagus) as is seen in achalasia.
- Swallowing electromyography
- Laryngeal EMG
- Manometry
These investigations are used to assess muscle activity, either with oropharynx or esophagus, to assess impairment of pharyngeal or esophageal motility.
- Transnasal laryngoscope
- Upper GI endoscopy
These investigations allow the doctor intraluminal visualization to assess the lining of the pharynx and esophagus. A fiberoptic endoscopic examination of swallowing utilizes a transnasal laryngoscope will assess pharyngeal swallowing. An upper GI endoscopy allows the doctor to assess the alimentary tract all the way from the pharynx to lower end of the esophagus.
References
- Dysphagia. Medscape
- Swallowing Disorders. NIH.gov