Bowel Prolapse (Rectum) Causes, Symptoms, Treatment
A prolapse can affect many organs of the body. It specifically affects those organs that are next to a hollow cavity and open to the outside of the body. A prolapse simply means that one organs slips into and protrudes through another. It mainly affects the female reproductive tract and rectum of the large intestine. A bowel prolapse (large intestine) is more correctly known as a rectal prolapse. It is more likely to occur in older people and 8 out of 10 people with a rectal prolapse are women. Overall, rectal prolapse is an uncommon condition.
What is a rectal prolapse?
Rectal prolapse is a condition where a part of the rectum protrudes through the anus. The rectum is the large part of the digestive system that comes after the colon. It is part of the large intestine (large bowel). There are different types of rectal prolapse – some may protrude through the anus while others pass through the anal canal but not out of the anus. Apart from elderly women being most affected, it also occurs in young children usually within the first 3 years of life.
Rectal Prolapse vs Hemorrhoids
The difference between a rectal prolapse and hemorrhoids can sometimes be confusing. These are two different conditions. One type of prolapse discussed below (mucosal prolapse) can be a consequence of long-standing hemorrhoids. In rectal prolapse, the a portion of the rectal wall protrudes through the anus.
In hemorrhoids, it is the inflamed veins that may protrude through the anus. It may also develop under the skin around the anus. Straining to pass stool over a long period of time can increase the risk of hemorrhoids and rectal prolapse. Although both conditions affect the same area, the rectum, and have the same symptoms it is important to remember that these are two separate conditions entirely.
Types of Rectal Prolapse
The rectum constitutes the last 12 to 15 centimeters (about 5 to 6 inches) of the large intestine. Its main function is to hold feces particularly before a bowel movement. Feces pass from the rectum, down the anal canal and out of the anus into the environment. The rectum has a thick wall comprising three layers. The inner layer of the rectum contains a mucosa that is similar to the rest of the large intestine. There are three types of rectal prolapse:
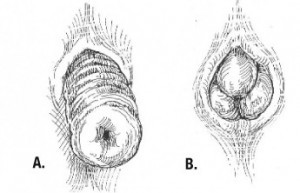
- Full thickness prolapse is where a portion of the rectal wall protrudes through the anus and this includes the entire thickness (all 3 layers) of the wall.
- Mucosal prolapse is where the inner layer of the intestinal wall (mucosa) pulls away from the rest of the wall and protrudes through the anus.
- Internal intussusception is where one part of the rectum folds into itself (telescoping) and may enter the anal canal but does not protrude out of the anus.
Pictures of rectal prolapse – full thickness (A) and mucosal (B)
Causes of Rectal Prolapse
The exact cause of a rectal prolapse is not completely understood. However, several risk factors have been identified. There are theories as to why a rectal prolapse may occur:
- A weakening in the pelvic floor and related disturbances allows a sliding hernia to develop in the rectum, which gradually progresses to become a full thickness prolapse.
- A full thickness prolapse essentially starts as internal intussusception (also a type of prolapse). Long term straining contributes to the intussusception (telescoping) becoming a full thickness prolapse.
- The connective tissue attaching the rectal mucosa to other layers of the rectal wall becomes loose and stretched. Over time this internal layer pushes through the anal canal and anus in what is termed as a mucosal prolapse.
Risk Factors
There are a number of risk factors associated with a rectal prolapse. These factors are not the cause of a rectal prolapse but instead increase the risk of it occurring. Not every person with one or more of these risk factors will definitely develop a rectal prolapse.
- Straining to defecate in chronic constipation.
- Long term diarrhea.
- Pregnancy and childbirth.
- Previous surgery, especially to the pelvic region.
- Pelvic floor dysfunction, especially in the elderly.
- Cystic fibrosis.
- Malnutrition.
- Deformities in bowel development.
- Neurological conditions (sometimes) – multiple sclerosis (MS), injury to the lower back and pelvis, lumbar disc disease and tumors of the spine.
Signs and Symptoms
The signs and symptoms may vary depending on the severity and type of prolapse.
Appearance
The main feature in a full-thickness or mucosal prolapse is bright red tissue (like a lump or swelling) protruding through the anus. In the early stages the tissue may recede after a bowel movement or can be pushed in manually. These may not be the first signs and symptoms to develop. This protruding tissue will not be visible in internal intussusception.
Sensation
The sensation of not being able to empty the bowels completely and the frequent urge to pass stool is usually present. It is sensation of fullness like there is a foreign body in the rectum, even after having a bowel movement. Anal pain, itching and burning may also be present to varying degrees.
Stool
Patients may pass stool very frequently and it is usually small amounts at a time. There may also be blood in the stool, or bleeding from the anus even without a bowel movement. Among the first symptoms of rectal prolapse are leakage of stool (fecal incontinence) with/without mucus and blood. Often a person soils their underwear.
Treatment of Bowel Prolapse
There are no specific drugs to treat a bowel (rectal prolapse). In fact children may not require treatment and the condition can resolve on its own. In the early stages, for both children and adults, simple dietary and lifestyle measures may be sufficient. However, as the condition progresses and especially in full-thickness prolapse, surgery may become necessary. The approach to treatment should be decided upon by a doctor in consultation with the patient. A prolapse should not be ignored even if it can be easily pushed back into the anus.
Diet and Exercise
A high fiber diet with plenty of water may help to alleviate constipation. This can reduce straining and slow down the progression of the prolapse. Stool softeners may be prescribed to assist with relieving constipation and straining during a bowel movement. Kegel exercises may be beneficial in strengthening the pelvic floor muscles, and therefore the support for holding the rectum in place.
Pushing Back Prolapse
Pushing back the prolapsed tissue as soon as possible can help the condition resolve without surgery. It is not always an effective means of treating the condition and should be only done if a doctor approves doing so. Straining or any other action that causes the tissue to protrude should also be avoided.
Surgery
Surgical intervention is reserved for severe cases. It is the only effective option for a full thickness prolapse. The decision to operate depends on a host of factors and is decided upon on an individual case basis. There are two surgical approaches – either through the abdomen (abdominal procedures) or around the prolapse (perineal procedures).
References:
emedicine.medscape.com/article/2026460-overview
www.bupa.co.uk/individuals/health-information/directory/r/rectal-prolapse
www.webmd.com/digestive-disorders/tc/rectal-prolapse-topic-overview