Colonoscopy – Preparation, Procedure, Pictures, Risks, Cost
What is a Colonoscopy?
Colonoscopy (Greek kolon = large intestine; skopein= to watch) is a diagnostic procedure during which a doctor – usually gastroenterologist – inspects the inner lining (mucosa) of your colon and rectum by a flexible viewing tube – colonoscope – that has a camera and light on the end (Picture 1). Colonoscopy may be done in a hospital or in an outpatient office.
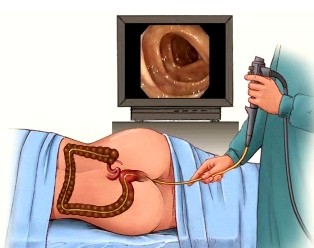
Picture 1. Colonoscopy
Hemorrhoids, diverticula, bleeding, polyps, tumors (colorectal carcinoma, lymphoma), inflamed mucosa, ulcers or fibrous tissue can be detected in the colonic or rectal mucosa. Few inches of the last part of the small intestine ,commonly affected by Crohn’s disease, can be also checked.
When Is a Colonoscopy Ordered?
Colonoscopy may be done in (1,2):
- Unexplained iron deficiency anemia to find an eventual source of bleeding in the large intestine
- Blood in the stool – to find the source of bleeding and treat it
- Unexplained chronic diarrhea – to find eventual inflammation in the colon (colitis)
- Unexplained abdominal pain
- Unexplained sudden weight loss – to find a cause like inflammatory bowel disease or colorectal cancer
- Inflammatory bowel disease to monitor its progress and treat eventual complications
- Abnormal result of a X-ray with barium enema to confirm suspected disorder of the colon
- Twisting (volvulus) of sigmoid colon – to resolve it
- Individuals after 50 with no risk factors for colorectal carcinoma; after 40 if they have family history of colorectal carcinoma; in adolescence if there is a hereditary type of carcinoma in the family.
Colonoscopy Preparation
Few weeks before a colonoscopy, your doctor will discuss with you about the following issues:
1. Relative Contraindications for a Colonoscopy
Unless important reason exists, a colonoscopy should not be done in (3):
- Pregnancy
- Acute heart disease
- Bowel perforation or complete obstruction
- Acute diverticulitis
- Fulminant colitis, toxic megacolon, colonic necrosis
- Acute peritonitis
- Abdominal aortic aneurysm larger than 5-6 cm and causing symptoms
- A disorder of blood coagulation or significantly lowered leukocytes or platelets in the blood
- Bochdalek hernia
- Non-cooperative or non-treatable patient
2. Drugs and Procedures Not Allowed Before Colonoscopy
A week before the procedure (or as doctor instructs) the following should not be taken:
- Aspirin and drugs for arthritis (ibuprofen, naproxen, etc.), because they may cause intestinal bleeding
- Iron pills, because they may make stool hard and hard to clean out during colon cleansing
- Barium swallow or enema, because barium can cover intestinal mucosa thus hiding it from doctor’s view
- Blood thinning drugs (anticoagulants) – doctor should give proper instructions, do not make any action on your own
- Insulin should not be taken during fasting
Doctor will also ask, if you are allergic to some drugs including sedatives and anesthetics.
3. Foods to Eat and to Avoid Before Colonoscopy (Bowel Cleanse)
Your doctor should give you exact written instructions about how to prepare your bowel for a colonoscopy.
- 1-2 days before a colonoscopy you may drink only clear liquids (water, tea, clear juices, popsicles, gelatin (such as Jell-O) and eat no solid foods. Red or purple drinks should be avoided, since they may look as blood in the intestine. Alcohol is not allowed.
- At the evening before a colonoscopy, take a laxative ( a salty drink you have gotten from your doctor). This will make you visit bathroom several times during the night. No solid foods should be eaten after the laxative, and complete fasting is needed for 6-8 hours before the procedure.
- An hour or so before the procedure a doctor may give you an enema to completely clean your colon.
4. Have Someone with You
Arrange, that someone will drive you home after the procedure, since you will be not allowed to drive.
5. Agreement
Before colonoscopy you will need to subscribe a consent with which you agree to have a colonoscopy and declare that you are aware of its risks.
6. Sedation
In the hospital or outpatient office, you will usually get a mild sedative as an injection into a vein, which will make you drowsy. You will be aware of the procedure but often you won’t be capable to communicate with the doctor. No sedation, or complete anesthesia are also possible. When extensive inflammation of the colon, or biliary tract disorders are expected, larger dose of sedatives may be given to prevent pain.
Colonoscopy Procedure
You will lie on the examining table on your left side and doctor will check your rectum with a gloved finger for eventual obstruction. Doctor will then administer the colonoscope through your anus into the colon and gently advance it toward the end of the colon. Then he will slowly pull the colonoscope out while observing the inner side of the colon. If necessary, doctor will perform a biopsy (cut some small pieces of colonic tissue for further investigation), stop the bleeding or remove the polyp. Investigation lasts about 30-45 minutes or more, depending on what needs to be done.
How Does It Feel?
Many patients are not even aware of the procedure after they wake up from sedation. You may experience some cramping and urge to defecate (but you will have an empty bowel so this is not a problem). Rarely, some patients experience pain to the point where procedure must be discontinued.
After the Procedure
After investigation, you will rest for about an hour or two to completely wake up. After discussion with the doctor, you may go home. You may experience some cramping or bloating (due to inflated air during the procedure) for the next day or two.
Results
Right after the procedure, doctor can tell you what he has seen and what procedures or treatment he has performed. Biopsy samples are sent to pathology laboratory and doctor can inform you about results in a week or so.
Complications
Colonoscopy is generally a safe procedure and complications are rare (2):
- Bleeding may appear (and in most cases can be stopped) during the procedure or as late as a week later; it usually stops spontaneously but sometimes another colonoscopy is needed.
- Arrhythmia, mostly due to side effect of sedatives
- Small bowel obstruction
- Diverticulitis
- Colon perforation
- Possibility of transmission of a disease from one patient to another is practically excluded. Sedatives may cause anxiety, nausea, allergy or respiratory depression.
- Rupture of the spleen is extremely rare
Flexible Sigmoidoscopy
In flexible sigmoidoscopy only the last 60 cm of the colon (rectum, sigmoid and descending colon) is investigated. Procedure is used in pregnancy instead of colonoscopy, whenever only changes in distal colon are expected, and as screening for early signs of colorectal cancer. Preparation is with clear liquids a day before, and cleansing enema right before the procedure, which lasts 10-20 minutes. Complications are rare.
Virtual Colonoscopy (CT Colography)
Virtual colonoscopy (VC) is performed on a computer from CT images of the colon (4). It is used in patients that are not able to undergo classical colonoscopy or they refuse it. The same colon prep is needed as in conventional colonoscopy, and the air has to be inflated into a colon before CT images are taken; the procedure takes about 10 minutes. No sedation is needed, and colonoscope is not used. VC may be used as a screening for colorectal cancer, since it can provide clear images of small changes throughout entire colon. The procedure is expensive, not regularly available, there is no less discomfort as during conventional colonoscopy, no therapeutic intervention is possible, and there is considerable exposure to radiation.
Average Cost of a Colonoscopy
Currently, average cost of colonoscopy is:
- About $3,000 if not covered by health insurance (5)
- Zero to about $1,000 for patients with symptoms or risk factors that warrant health insurance (5)
- $400-800 for virtually colonoscopy (usually not covered by Medicare or health insurance) (6)
Cost of colonoscopy may greatly depend on the country, hospital, health setting expenses and cost of anesthesia.
When and How Often Should One Have a Colonoscopy?
General recommendations are (2):
- A person with average risk for colorectal cancer: first colonoscopy at 50 years of age and then every 10 years
- A person with increased risk (family history) for colorectal cancer: first colonoscopy at 40 years of age and if no polyps found, a colonoscopy every 5 years
- After removal of a large (> 2cm) sessile (flat) polyp, another colonoscopy in 3-4 months
- After removal of a non-cancerous polyp, another colonoscopy after 3 years
- After removal of multiple non-cancerous polyps, another colonoscopy after 1 year
- Before surgical removal of a colorectal cancer
- A person with family history of familiar adenomatous polyposis (FAP): colonoscopy or sigmoidoscopy at 10-12 years of age and then every year until 30-40 years of age
- Patients with long term Crohn’s disease: colonoscopy every 1-2 years
Related Articles:
- Upper Endoscopy Procedure, Video
- Crohn’s Disease Symptoms
- Diagnostic Imaging of the Abdomen (CT, X-Ray, Ultrasound, MRI)
- Ischemic Colitis
References:
- Colonoscopy indications (cigna.com)
- Colonoscopy complications (emedicine.com)
- Virtual colonoscopy (emedicine.com)
- Is colonoscopy expensive? (costhelper.com)
- Virtual colonoscopy (scandirectory.com)
