Bleeding In The Bowels, Causes, Symptoms, Tests, Treatment
It is not uncommon for there to be bleeding within the bowels. Most of the time it is very short lived and you would never notice it. The body quickly plugs up the site of the bleeding, which is usually minor, and there is no threat to a person’s health. However, massive or persistent blood loss in the bowels needs to be investigated further and treated. Not only can the blood loss be substantial but it may also be a sign of a very serious condition, like cancer in the digestive tract.
How to spot bowel bleeding?
Blood loss can occur from anywhere in the gastrointestinal tract – from the mouth to the anus. When it occurs in the upper gastrointestinal tract, then it may be visible if vomiting occurs. Otherwise the bleeding may be detected in the stool. Bleeding in the lower gastrointestinal, most of the small and large intestines (bowels), is only detectable in the stool. However, in most instances the blood loss is so minor that it is not visible to the naked eye. There is no significant change in stool color or blood in the toilet water after defecation.
For this reason blood in the stool has to be detected with laboratory tests, like the fecal occult blood test (FOBT). The name of this test simply means minute amounts of blood (occult blood) in the stool (feces). It is not routinely done unless bleeding in the bowels is suspected. Bleeding from the anus, where there is blood upon wiping after passing stool, reddish discoloration of the stool or blood in the toilet water is usually due to conditions like hemorrhoids (piles). It needs to be treated but it not a serious condition.
Causes of Bleeding in the Bowels
There are a number of reasons why blood loss may occur in the bowels. Firstly it is important to understand what is meant by the term ‘bowels’. It refers to the intestines, both small and large. This starts where the stomach ends and continues until the anal canal. The small intestine is responsible for the digestion and absorption of nutrients. The large intestine is where stool is formed and most of the water in the gut is reabsorbed.
The walls of the bowels are thick and contain muscle cells that contract and relax to move the contents within it. The wall is also well vascularized to ensure adequate blood supply to nourish the surrounding tissue and carry nutrients absorbed from the bowel to the liver. If there is a break in these vessels then blood can leak out into bowel cavity. If the bleeding is higher up in the bowels then it may degrade and darken by the time it is passed out in the stool. Some blood can be digested as well.
Common Causes
A number of conditions can cause bleeding in the bowels but the more common of these include:
- Peptic ulcer disease when open sores form in the wall of the upper gut. The duodenum (small intestine) is the most common site for peptic ulcers but not all ulcers bleed. It is more likely to arise with an H.pylori infection or excessive use of certain drugs.
- Hemorrhoids is a common condition of the rectum and anus. The veins here become swollen and inflamed resulting in itching, burning, pain and sometimes bleeding.
- Diverticulitis is very often seen in the elderly. Outpouchings form in the colon (diverticula) which can become infected every now and then.
- Inflammatory bowel disease (IBD) is an autoimmune condition where the bowel wall becomes inflamed and ulcerated. Certain types like Crohn’s disease can occur anywhere in the digestive tract.
- Cancer is a malignant growth that can occur anywhere in the body. The bowels, particularly the colon and rectum, are two common cancer sites. It is only when bleeding occurs from the cancer that blood will be found in the bowels.
It is important to note that although cancer is listed as a common cause for bleeding in the bowels, the other four conditions should first be excluded as they usually occur more frequently.
Less Common Causes
The less common causes of bleeding in the bowels include:
- Anal fistula
- Arteriovenous (AV) malformations
- Alcohol abuse
- Bleeding disorders
- Gastritis (erosive)
- Infectious colitis
- Mallory-Weiss tear
- Pancreatitis
- Poisoning (ingested toxins)
- Polyps
- Trauma
Signs and Symptoms
As mentioned above, bleeding in the bowels may not be overtly obvious. Bleeding is a symptoms and other symptoms that occur as a result of blood loss may be easier to identify at the outset.
- Dark, tarry stools (melena) sometimes with an unusual odor due to blood in the stools.
- Gross blood visible when wiping, in feces and toilet water or soiling underwear.
- Anemia as a result of massive blood loss suddenly or slow blood loss over a period of time.
- Paleness of the skin, fatigue and shortness of breath due to anemia.
- Itching, burning and/or pain, and feeling of incomplete bowel movement occurs in hemorrhoids in particular.
Other signs and symptoms may also be present depending on the underlying cause of bleeding in the bowels.
Tests and Treatment
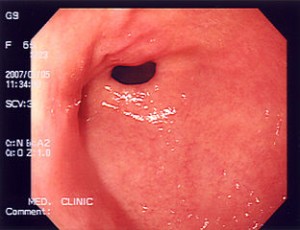
When intestinal bleeding is suspected, a doctor may request several diagnostic investigations to confirm the presence of blood in the stool and then to identify the cause. A stool analysis involves testing for blood in the stool, as well as microbes and parasite eggs, white blood cells, proteins and antibodies. The test to attempt to identify the presence of blood is known as the fecal occult blood test (FOBT). A colonoscopy to visualize the large intestine, enteroscopy for the small intestine or an upper GI endoscopy to examine the upper digestive tract may be done to identify the site of bleeding. A host of other laboratory tests and imaging studies may also be conducted.
The treatment for bleeding in the bowels varies depending on the cause. It may involve a combination of medication, dietary and lifestyle changes as needed for the condition in question. For some of these conditions, surgery is the only treatment. Surgery is also sometimes to stop the bleeding, irrespective of the cause. Cauterization using an electric current can “seal” the bleed but it may not be a permanent solution to the problem. It may be done during an endoscopy, enteroscopy or colonoscopy. However, the underlying condition needs to be treated appropriately in order to prevent future bleeds.