Cardiac Output (Heart Pumping Ability) Low and High Causes
Blood is constantly flowing through the heart. The right side of the heart receives low oxygen blood, sends it to the lungs for oxygenation and the left side then pushes out this oxygen-rich blood to the rest of the body. However, the quantity of blood and the time over which this happens also matters. The heart has to be able to receive sufficient blood and push out enough to maintain oxygen supply throughout the body. This is necessary for life.
What is cardiac output?
Cardiac output is the quantity of blood that is pumped out of the heart in a minute. It is calculated by the heart rate (beats per minute) multiplied by the stroke volume (amount of blood pushed out of the heart upon contraction). If the cardiac output is too low then the body does not receive enough oxygen to function properly.
In certain diseases, the heart function may be affected and this may reduce cardiac output. The heart will try its compensate and maintain a normal cardiac output (compensatory mechanisms). However, after time it is unable to do so. Cardiac output is ultimately reduced and this state is an indication of heart failure.
How much blood does the heart pump?
The amount of blood that the heart pumps in a minute (cardiac output) varies among individuals. This depends on various factors. For example, the heart has to pump more blood during exercise because the body’s oxygen demand increases. The average adult heart pumps about 3 to 4 liters of blood per minute when a person is at rest. This can increase by several times when during strenuous exercise.
What happens in cardiac output?
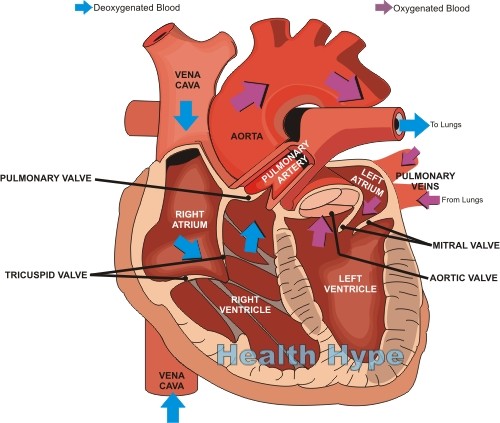
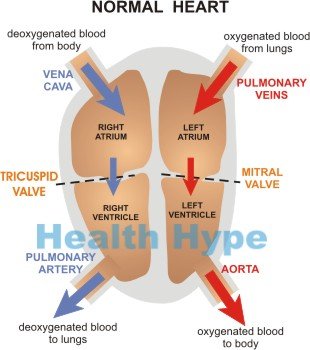
The heart is a muscular pump. It has thick muscles that make up the walls. It can stretch to accommodate blood but can also contract with force. This ensures that the heart is constantly pushing out blood to the body. At rest (diastole), blood from the body or lungs fills into the atria (singular ~ atrium). There are two atria – the right atrium and left atrium.
The right atrium receives low oxygen blood from the body and the left atrium receives oxygen-rich blood from the lungs. This blood from the atria then enter the ventricles. When the heart contracts (systole), the blood is pushed out of the ventricles and sent out to the lungs and body.
The right ventricle sends the low oxygen blood to the lungs for oxygenation. The left ventricle sends oxygen-rich blood to the rest of the body. This process (cardiac cycle) is carefully coordinated to ensure that the heart can work at its peak without unnecessary strain on the heart muscle. There are a number of factors to consider in cardiac output.
Cardiac Output Terminology
A doctor will request tests when there is a heart disease or suspicion of heart disease. These tests may reveal whether the cardiac output is affected or not. There may be no symptoms although cardiac output is affected. It is important to understand some of the medical terms related to cardiac output.
- Stroke volume is the amount of blood pushed out of the heart upon contraction.
- End-diastolic volume is the amount of blood that fills in the heart after relaxation and just before the next contraction.
- End-diastolic pressure (preload) is the pressure present before a contraction. It indicates the extent of cardiac muscle stretching and determines the force at which the blood can be pushed out during contraction.
- Myocardial contractility is the ability of the heart muscle to push out blood upon contraction. It is essentially the strength of the heart muscle to produce force.
- Systolic aortic pressure is the pressure of the blood that is pushed out of the heart which will be at its greatest immediately after the blood leaves the heart and enters the aorta.
Stroke volume and systolic aortic pressure is a combination of end-diastolic volume, end-diastolic pressure and myocardial contractility. If any of the above factors are affected or impaired, the cardiac output can be reduced. This means that the sufficient blood will not be circulated throughout the body at a pressure that will maintain a healthy circulation and perfusion.
What is Windkessel Effect?
Oxygen-rich blood from the left ventricle is carried out of the heart by the aorta. It is the largest artery in the body. The aorta is elastic and will stretch as high pressure blood leaves the heart. It then contracts back to its normal size once the blood passes.
The recoil of the aorta will then play a further role is keeping the blood flowing at the correct pressure. This prevents the heart from having to pump blood at an excessively high pressure. This is known as the “Windkessel Effect”.
What is Starling’s Law of Heart?
This law states that in a healthy heart with normal cardiac output, the amount of blood that is pumped out of the heart (stroke volume) should return in full (end diastolic volume). The greater the volume of blood that leaves the heart, the greater the volume that will return and vice versa. If less blood returns that what was pushed out, then the cardiac output will decrease. This is an important concept to understand in order to identify the type of heart failure and identify the cause of reduced cardiac output.
Causes of Low or High Cardiac Output
A low cardiac output is a problem because the body may not be receiving sufficient oxygen for its needs. At the other end, a high cardiac output can also be dangerous as it can lead to heart strain with a host of serious complications.
Low Cardiac Output
Any heart disease where the heart function is reduced may lead to low cardiac output. This includes:
- Myocardial infarction (heart attack)
- Cardiomyopathy
- Heart failure due to various causes.
- Excessive blood loss.
- Sepsis (“blood poisoning”)
High Cardiac Output
- Anemia
- Hyperthyroidism
- Sepsis (sometimes)
It is important to note that cardiac output can be affected by various ways even when the heart is healthy. From hormones to nerve impulses, heart activity is determined by a host of factors. Therefore cardiac output can suddenly change when there is disturbance elsewhere in the body which has an effect on the cardiovascular system.