Ischemic Heart Disease (IHD) – Lack of Blood Supply and Oxygen
The heart has thick walls mainly composed of muscle in order for it to maintain its functioning of pumping blood throughout the body. This muscular layer is known as the myocardium and surrounded by the inner lining (endocardium) and outer layers (epicardium). The heart is working throughout life, contracting and relaxing, to ensure that blood is constantly in circulation.
Muscle cells in general are demanding of both oxygen and nutrients and the myocardium is no different. Although the heart is the central organ of circulation, the myocardium does not derive its oxygen supply from within the heart but is instead dependent on the coronary arteries for a constant flow of oxygen and nutrients. When any part of the body is deprived of an adequate blood supply, yet still has a sufficient flow to sustain life, it undergoes injury known as ischemia. In terms of the heart muscle this is known as myocardial ischemia.
What is ischemic heart disease?
Ischemic heart disease (IHD) is a group of disorders where there is an inadequate blood supply to the heart muscle leading to myocardial ischemia. A diminished blood supply means that heart muscle cells receive less oxygen and nutrients needed to function optimally and waste products manufactured is not drained away in an efficient manner.
The term ischemic heart disease is often used synonymously with coronary artery disease (CAD) or coronary heart disease (CHD) because an obstruction of the coronary arteries is the single most common cause of myocardial ischemia. However, with systemic disturbances like shock there is a reduction in blood supply and oxygen to the entire body although the coronary arteries are normal and healthy. Shock can also cause myocardial ischemia and is also considered as a cause of ischemic heart disease but is not associated with coronary artery disease.
Ischemia heart disease may present as many clinical syndromes including :
- Angina pectoris (angina heart pain)
- Myocardial infarction (heart attack)
- Chronic IHD with heart failure
- Sudden cardiac death
How does IHD occur?
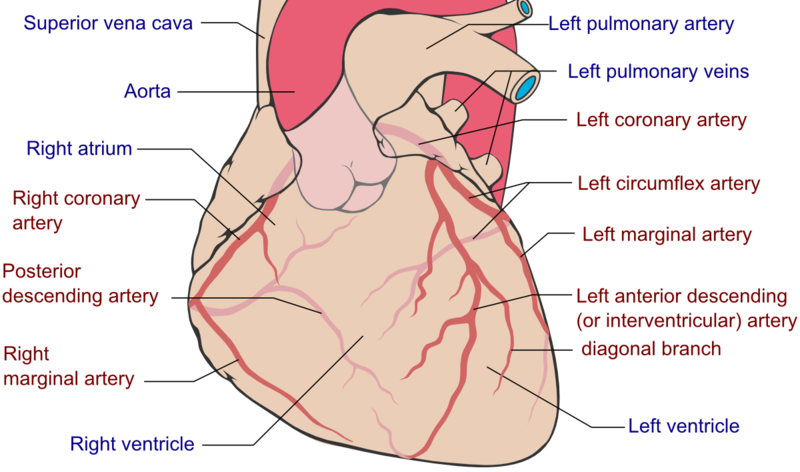
About 90% of IHD is due to coronary artery occlusion. There is two coronary arteries – left and right – both of which arise from the aortic sinus, a dilated part of the aorta just above the aortic valve. These arteries are mainly narrowed by the development of atherosclerotic plaques in its wall (atherosclerosis) which develops gradually over time. It may be further compounded by blood clots that develop at the site (thrombus). The coronary arteries, like any other artery, may also experience vasospasm, where the muscles in its wall contracts to a large degree and narrows its lumen. Any one or more of these factors will reduce the blood flow to the heart wall and therefore deprive the cells of oxygen and nutrients.
Picture of Coronary Arteries from Wikimedia Commons
Ischemia is the damage to the cells that occurs with a reduce blood supply and not solely from oxygen deprivation (hypoxia). However, cells cannot survive without oxygen for just a few minutes and injury sets in within seconds, unlike with lack of nutrients or accumulation of wastes. Therefore much of the damage in the short term is due to a lack of oxygen. If an artery is less than 75% blocked then a person may be asymptomatic. The onset of symptoms is associated with increased demand by the heart muscle like during exercise or other strenuous activity.
Myocardial ischemia may cause episodes of cardiac pain associated with activity which is known as angina pectoris, where there is no death of cells. If a clot forms when the atherosclerotic plaque ruptures, the blood flow is severely compromised and muscle cells in an area may die known as myocardial infarction (heart attack). Sometimes a part of the heart may experience constant myocardial ischemia even without increased cardiac demand and this can disrupt the electrical activity of the heart and lead to sudden cardiac death. Long term myocardial ischemia and changes in unaffected heart muscle after an infarct leads to heart muscle disease (ischemic cardiomyopathy). It affects the ability of the heart muscle to function optimally and leads to heart failure which is termed chronic IHD with heart failure.
Causes of Ischemic Heart Disease
As mentioned above, most cases are due to atherosclerosis which is the development of fatty plaques in the wall of the coronary arteries. Atherosclerosis is associated with risk factors such as :
- Hypertension – high blood pressure
- Hyperlipidemia – high levels of fats (cholesterol, triglycerides) in the blood
- Cigarette smoking
- Diabetes mellitus
Additional risk factors include :
- Advancing age
- Family history
- Gender – men at a higher risk
- Obesity
- Sedentary lifestyle
Signs and Symptoms
The signs and symptoms of ischemic heart disease depends on the clinical syndrome it presents as. The common features are cardiorespiratory manifestations.
Ischemic cardiac pain is the term for pain originating from injury to the heart wall associated with reduced blood supply. It is typically described as pain having the following characteristics :
- Located at the center of the chest.
- Radiates to the arm, neck and/or jaw.
- Provoked by exercise and stress and relieved by rest.
- More likely to arise after a large meal and exposure to cold wind.
- Dull, constricting, choking heaviness, squeezing, burning and/or crushing.
- Begins during exercise and gradually worsens but is unlikely to arise after exercise.
- Associated with shortness of breath, nausea, vomiting, sweating, dizziness and/or fainting.
Many other non-cardiac causes may cause a similar type of chest pain and it is therefore important to differentiate between cardiac and non-cardiac chest pain. Similarly it is essential to differentiate between angina and heart attack pain in order to seek immediate medical attention for the latter.
The clinical features associated with heart failure arises gradually over time. This includes :
- Difficulty breathing when lying flat and with activity.
- Swelling of the ankles and feet and abdomen as the condition progresses.
- Fatigue
- Weakness
- Dry cough
- Palpitations
- Loss of appetite
- Difficulty sleeping for long periods and awakening with breathlessness