Pelvic Inflammatory Disease (PID) Causes, Symptoms, Treatment
Female infertility is a relatively common problem. About 1 out of 10 females of reproductive age either cannot fall pregnant or carry the pregnancy to term. There are a host of different causes of infertility among males and females. One of the leading causes of female infertility is pelvic inflammatory disease (PID).
What is pelvic inflammatory disease?
Pelvic inflammatory disease (PID) is a condition where the female reproductive organs (uterus, fallopian tubes, ovaries and adjacent structures) become inflamed usually due to an infection. It is a serious complication of common sexually transmitted diseases (STDs) like chlamydia and gonorrhea. Pelvic inflammatory disease is one of the leading causes of infertility among women.
Overall episodes of pelvic inflammatory disease (PID) occur in about 1 million women in the United States. Females under 25 years of age are the highest risk group, particularly those who have multiple sex partners and do not use contraception. With infections like chlamydia being the most common among teens, pelvic inflammatory disease (PID) is understandably more frequently seen in this age group.
Causes, Risks and Spread
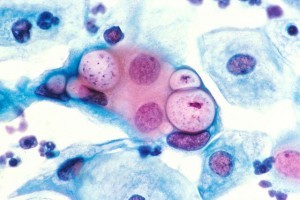
A number of different bacteria can cause pelvic inflammatory disease but N.gonorrhoeae and C.trachomatis, bacteria responsible for gonorrhea and chlamydia respectively are the most common causes. Other pathogens that can also cause pelvic inflammatory diseases includes:
- Cytomegalovirus (CMV)
- Escherichia coli
- Gardnerella vaginalis
- Haemophilus influenzae
- Herpes simplex virus 2 (HSV-2)
- Mycoplasma hominis and Mycoplasma genitalium
- Peptococcus species
- Streptococcus agalactiae
- Trichomonas vaginalis
- Ureaplasma urealyticum
The infection progresses through two stages:
- Entry of the pathogen into the vagina with infection of the vagina that may extend up to the cervix. Usually the pathogen is restricted by the cervical mucus from entering the uterus. The pathogen may cause a vaginal or cervical infection without progressing further and will therefore not cause pelvic inflammatory disease.
- Passage of the pathogens into the uterus and eventual spread to the fallopian tubes and even the ovaries. Vaginal and cervical inflammation may weaken the cervical mucus barrier and intercourse may push the pathogen beyond the cervix into the uterus.
Inflammation of these infected structures can lead to scar tissue formation. This scar tissue can cause an obstruction in the fallopian tube and prevent sperm from reaching the egg cells or even result in an ectopic pregnancy as the egg cell is ‘stuck’ in the fallopian tube.
There is some evidence that certain people may have a genetic susceptibility to chlamydia. These genes alter the body’s innate immune response to the bacteria. As a result complications like PID may occur. However, exposure to chlamydia bacteria, mainly from sexual contact, is still necessary for an infection to occur.
Spread of Pelvic Inflammatory Disease
Pelvic inflammatory disease is a complication of a sexually transmitted disease (STD). The infection usually starts in the vagina and spreads upwards into the uterus, to the fallopian tubes and eventually reaches the ovaries. Sexual contact is the most likely way that these bacteria which cause pelvic inflammatory disease is spread. However, it can also enter with IUDs (intra-uterine devices), during childbirth, with an abortion or as a result of a miscarriage.
Risk Factors for Pelvic Inflammatory Disease
Some people are at a greater risk of contracting the microorganisms that can progress to pelvic inflammatory disease. This includes:
- Being a woman 25 years or younger.
- Having multiple sexual partners or one partner with multiple sexual partners.
- Not using barrier protection like condoms.
- History of a sexually transmitted disease (STD) or pelvic inflammatory disease (PID).
- Douching regularly.
Signs and Symptoms
Sometimes pelvic inflammatory disorder (PID) presents with little to no symptoms. Chlamydia is a common pathogen that presents with mild symptoms in pelvic inflammatory disease (PID) and sometimes there is an absence of any symptoms altogether.
Pain
Pain is one of the main and most prominent symptoms. It includes pain during intercourse, when urinating as well as lower abdominal pain and pelvic pain. The intensity of the pain can vary and this is not a clear indication of severity. Sometimes it can be very severe pain while at other times it may be just a dull ache.
Other
There may also be other symptoms apart from pain. This includes:
- Abnormal vaginal bleeding
- Abnormal vaginal discharge
- Offensive-smelling vaginal secretions
- Fever
- Vomiting (severe cases)
Treatment for PID
Antibiotics is the main course of treatment for pelvic inflammatory disease. It needs to be started as soon as possible and the entire course needs to be completed to effectively treat the infection. Sometimes a combination of antibiotics are prescribed until a culture test of a sample of the vaginal discharge indicates the exact causative organism. The antibiotic prescription may then be adjusted accordingly.
Re-infection is not uncommon particularly when barrier protection is not used. Therefore the partner(s) of a women with pelvic inflammatory disease needs to also be treated. While abstinence from intercourse is advised until the infection resolves, a new infection can set in if the partner is not treated. Apart from infertility as a complication, about 1 out of 4 cases of pelvic inflammatory disease may lead to chronic pelvic pain.
Prevention of PID
In a large number of cases pelvic inflammatory disease (PID) can be avoided by preventing the causative sexually transmitted infection. Early diagnosis and treatment of these infections will also prevent pelvic inflammatory disease. Some of the lifestyle measures that should be considered as a preventative measure includes:
- Using condoms during intercourse. This prevents not only semen but also the causative bacteria from entering the vagina. Other forms of contraception like birth control pills cannot prevent sexually transmitted diseases. During the first few weeks of IUD insertion, the risk of PID is higher and condoms must be used.
- Avoid intercourse, especially unprotected intercourse, with multiple partners. The risk increases with the number of partners. It is also important to remember that having a partner who has multiple partners can also increase the risk.
- Proper monitoring can also play a role in preventing PID after treatment. Younger women have a high risk of re-infection within 6 months of treatment. Regular monitoring will indicate an infection early and the necessary treatment can therefore be administered as soon as possible.