Periapical Abscess (Pus at Tooth Root)
What is a periapical abscess?
A dental abscess is a broad term used to describe an abscess in the tooth and structures around it. A periapical abscess is an inflammatory reaction with the accumulation of pus at the root of an infected tooth. It can lead to death of the central region of the tooth known as the dental pulp. Generally a periapical abscess is an acute dental infection requiring immediate dental intervention. The condition is associated with significant discomfort and extreme pain. If left untreated it can lead to various complication and permanent loss of the affected tooth. A periapical abscess is the most common type of dental abscess among children. Another type, a periodontal abscess, is where the abscess is located in the tissue around the tooth, including the alveolar bone. A periodontal abscess is more commonly seen among adults.
How does a periapical abscess form?
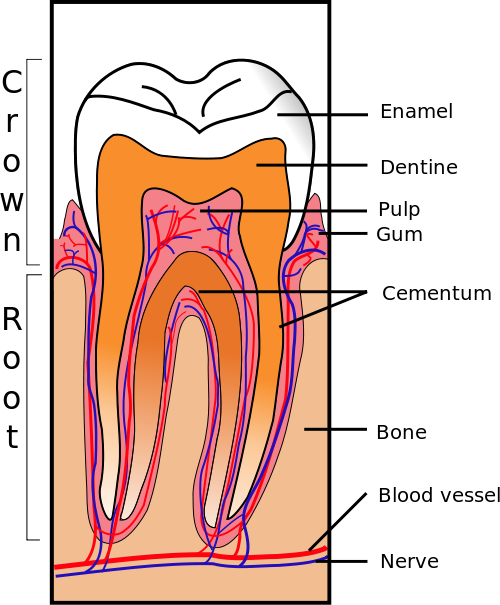
A tooth is composed of three layers of tissues at the crown (visible) portion namely enamel, dentin and pulp. Dental pulp is the vital portion of the tooth located below mineralized layers of enamel and dentin. The pulp is responsible for nutrition, nerve supply, blood supply and defense mechanism of the tooth.
Erosion of the outer harder layers of the tooth with entrance and proliferation of bacteria within the tooth cavity is known as dental decay. As the disease progresses, bacteria travel through enamel and dentin towards the dental pulp. Once the bacteria reach the dental pulp, an acute inflammatory response takes place within the pulp tissue. This reaction eventually leads to death of dental pulp causing loss of blood supply, nerve supply and defense mechanism of the tooth. The collection of white blood cells and pus is what is termed an abscess.
As the infections travels through the tooth root toward the alveolar bone, it forms an abscess at the apex of the tooth root. The abscess generally remains confined at the periapex due to defense mechanism of the alveolar bone. Once the bacterium crosses the barrier at the periapical region, it can spread within the bone and also towards other anatomical structures in proximity, possibly leading to a periodontal abscess.
Picture from Wikimedia Commons
Signs and Symptoms
A small periapical abscess may be asymptomatic apart from the history of tooth decay and pain associated with the decay itself. In most cases a dental abscess is associated with intense pain. The pain is often described as throbbing and sharp shooting in nature. The tooth becomes tender on pressure application and chewing from the affected side becomes difficult. The affected tooth is slightly extruded from its socket.
As the abscess is an acute inflammatory reaction, fever, chills and a general body ache is usually experienced. The lymph nodes on the affected side becomes enlarged and tender in nature. Periapical abscess usually forms an intraoral swelling, meaning swelling within the mouth. The affected gums become reddish, swollen and tender. As the abscess progresses, it causes a lump like swelling of the jaws. The swelling increases rapidly and is very tender and painful. The swelling often causes difficulty in opening the mouth and lead to facial asymmetry.
In few cases the abscess forms a channel leading to an opening over the gums or the skin, which drains the pus. The channel is known as a sinus tract, which leads to incomplete drainage of the pus and can cause a chronic periapical abscess.
Complications
An undiagnosed or untreated periapical abscess can lead to complications.
- A chronic periapical abscess can lead to dental cyst formation or diseases such as osteomylitis.
- In certain circumstances such as in immune compromised patients, the abscess can spread to vital organs.
- The abscess can lead to a condition called as Ludwig’s angina, characterized by cellulitis involving the floor of the mouth and sub mandibular spaces. The condition can lead to airway obstruction and is therefore potentially life threatening.
- In rare cases the dental infection can lead to septicemia, neck space infection, cavernous sinus thrombosis and maxillary sinusitis.
Causes and Risk Factors
The bacteria involved in formation of periapical abscess include Streptococcus viridians, Prevotella and Fusobacterium. These infections are more likely to arise in cases of tooth decay and dental cavity formation. Here the bacteria gain entry through the opening to the mouth. However, sometimes the bacteria may reach the site via the bloodstream.
Infant Feeding
Various feeding practices play a significant role in the development of cavities in infants. This is known as early childhood caries (ECC) and affects both bottle fed and breastfed infants. It is a combination of prolonged feeding at night and drinking fermentable carbohydrtes like fruit juices. However, even prolonged and very frequent feeding of breast milk can be responsible. The infection is largely due to Streptococcus mutans and dental hygiene also plays a role in the condition.
Dental Hygiene
Poor or improper dental hygiene leads to the build up plaque. This is one of the main reasons for tooth decay in both adults and children. As plaque erodes the outer mineral layer of the teeth, it causes the formation of tiny holes that lead to the deeper layers of the tooth. Bacteria thriving on trapped food within these holes leads to tooth decay.
Tooth Injury
An infection can arise after injury to the tooth where its structure is compromised. Infections may even set in after dental surgery.
Gum Infection
A gum infection, gingivitis, can allow for bacteria to enter the root of the tooth and the pulp.
Other Infections
In rare cases, infections at other sites can spread to the inner tissue of the tooth. Bacteria may travel via the bloodstream to the teeth and this is known as hematogenous spread. It is uncommon as the immune system can usually limit the extent of the infection. However, in patients with a compromised immune system, this is more likely to occur.
Treatment
The treatment of a periapical abscess varies according to the extent, location, severity and duration of the abscess. The available tooth structure is also a chief factor in determining the treatment plan. A periapical dental x-ray is a must to determine the diagnosis as the lesion is similar to infected periapical granuloma or an infected dental cyst.
Root Canal
The lesions which are smaller in size are treated with a root canal procedure. The fine canals located in the root apex carry the blood vessels and nerves supplying the pulp. After the death of the pulp these canals are filled with bacteria and dead tissue. In a root canal procedure these canals are cleaned and infected material is removed.
In the subsequent dental visits the canals are irrigated with disinfectant solutions and sealed with suitable material. This procedure eliminates bacteria from the root canals. After complete removal of the bacteria from the canal, the abscess disappears as the nidus of the infection is removed. After sealing the canals a suitable material such as dental amalgam or dental composite is used to fill the prepared cavity to access the canals.
Medication
- Non-steroidal anti-inflammatory drugs (NSAIDs) are prescribed in conditions associated with pain. Medicines such as ibuprofen, naproxen, acetaminophen and diclofenac are prescribed to reduce the pain and inflammation.
- Antibiotics are generally not required for smaller lesions but are necessary for larger abscesses. Most commonly used antibiotics include amoxicillin, metronidazole and clindamycin.
Drainage
In cases with abscess involving buccal or submandibular spaces, antibiotic treatment followed by excision and drainage is advised. The excision can be intra-oral or extra-oral depending on the location and extent of the lesion. The procedure is carried out under local anesthesia.
Extraction
In a few cases the tooth associated with periapical abscess may be very extensively damaged as a result of tooth decay. Due to lack of restorable tooth structure it is not possible to carry out a root canal. Extraction of the affected tooth is the only option in such cases. The extracted tooth can then be replaced by a metal or ceramic bridge or dental implants.
References :
http://www.merckmanuals.com/home/mouth_and_dental_disorders/tooth_disorders/periapical_abscess.html
http://www.patient.co.uk/health/Dental-Abscess.htm