Gastroesophageal Reflux Disease (GERD) Causes and Acid Reflux Diet
What is GERD?
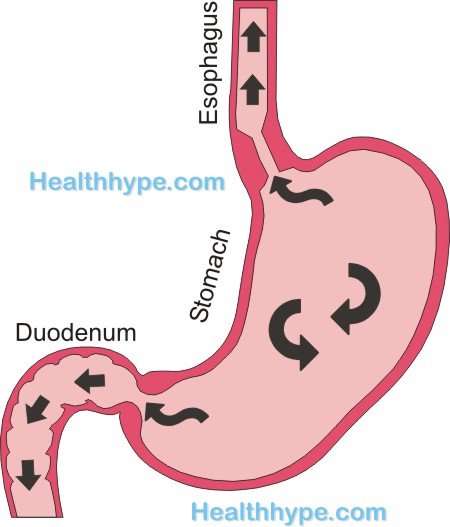
Gastroesophageal reflux disease (GERD) or gastro-oesophageal reflux disease (GORD) is the chronic form of acid reflux. Due to a number of reasons, the acidic stomach contents flow backward from the stomach into the esophagus (gullet). Since the esophagus is not structured to adequately handle the acid, GERD results in a number of symptoms or complications if left untreated.
Every person will experience acute bouts of acid reflux which often resolve spontaneously. These episodes are infrequent and usually triggered by certain factors like overeating or physical activity after a meal. With GERD however, the reflux is chronic – it occurs almost on a daily basis and sometimes even several times in a day.
How does GERD occur?
The lower esophageal sphincter (LES) prevents the acidic stomach contents from flowing out of the stomach and into the esophagus.
Most cases of GERD are associated with a dysfunction of the LES. This may occur for a number of reasons – in the acute setting, it is usually a result of certain foods and drinks like alcohol affect the tonicity of the sphincter but this is a temporary effect. With GERD however, the dysfunction is constant and just exacerbated by the same causes as acute acid reflux.
In some cases, the LES is functioning normally but due to various factors affecting the stomach, the LES cannot prevent the regurgitation. Sometimes bile from the duodenum also flows through the stomach and up into the esophagus.

Causes of GERD
The main cause of GERD is a lower esophageal sphincter dysfunction. This muscular valves is unable to remain contracted to the extent that it should and this allows the stomach contents to flow backward during stomach contractions and when lying flat. Other causes include :
- Hiatal hernia where a portion of the stomach protrudes through the opening in the diaphragm.
- Intra-abdominal pressure may also cause GERD and this commonly occurs due to abdominal obesity and pregnancy.
- Delayed gastric emptying is where the stomach contents do not exit the stomach at a normal rate and may back up into the esophagus.
- Impaired esophageal motility is a result of defective peristalsis that does not allow the regurgitated contents to be pushed back down and retained within the stomach.
Symptoms of GERD
Some cases of GERD remain asymptomatic for long periods of time and may only be detected by the complications, like those that arise in the upper respiratory tract, as explained under Silent Acid Reflux. The more common symptoms of GERD includes :
- Chronic heartburn (burning chest pain) especially after eating and at night when sleeping.
- Regurgitation
- Water brash which is a sudden collection of saliva in the mouth.
- Nausea and sometimes vomiting.
- Stomach ache or gastric pain, especially after eating.
- Stomach bloating which is a sensation of fullness or pressure in the stomach area.
Other symptoms that may be due to severe GERD :
- Chronic sore throat that tends to arise upon waking (morning sore throat) and eases during the course of the day.
- Difficulty swallowing (dysphagia)
- Lump in throat feeling
- Persistent cough
- Hoarse voice
What are the complications of GERD?
Over time, the irritation of the esophagus lining by the stomach acid may lead to a range of complications including :
- Esophageal ulcer
- Esophageal stricture
- Barrett’s esophagus
- Esophageal cancer
Prompt treatment may prevent complications.
What is the treatment for GERD?
Treatment involves the use of medication like :
- Antacids to neutralize stomach acid.
- Proton pump inhibitors or H2-blockers to reduce gastric acid secretion.
- Sucralfates to line the esophagus and protect it from the acid.
- Prokinetic drugs will speed up the movement of the stomach contents.
This is discussed further under stomach acid medication.
Laparoscopic anti-reflux surgery is rarely conducted but may be necessary in cases of persistent GERD that is unresponsive to medication.
Acid Reflux Diet
Acute acid reflux can be prevented by following the basic acid reflux diet tips below but in chronic cases related to gastroesophageal reflux disease or GERD, dietary management may only be useful in preventing acute exacerbations (flare ups).
GERD is associated with LES dysfunction (most common cause) as well as a hiatal hernia, increased intra-abdominal pressure and delayed gastric emptying. Therefore an acid reflux diet alone cannot treat GERD and has to be incorporated along with medication for proper management.
Acid reflux tends to aggravate at night and during sleep so the last meal of the day (usually supper/dinner) needs to be carefully monitored. The foods and drinks mentioned above should be avoided but if being consumed in moderation, it has to be avoided altogether in during supper/dinner.
Meal tips and eating habits that are important to consider include :
- Avoid eating large meals, especially at night. Small meals spread out throughout the day is preferable. Supper/dinner should be the smallest meal as the energy requirements are minimal at this time of the day.
- Focus on the meal by avoiding eating in front of the television. Being distracted tends to lead to overeating and eating too quickly which increases air swallowing (aerophagia) thereby contributing to excessive gas.
- Do not eat at least 2 to 3 hours before bedtime. Late night snacks have to be avoided altogether.
- Mild activity after a meal helps with gut motility. This may include a light stroll or even simple activities within the home. Never undertake any strenuous exercise or demanding physical activity as this can aggravate the reflux.
- Quit cigarette smoking and avoid even the occasional (social) smoke, especially after a meal. This includes cigar smoking.
- Avoid night caps and desserts laden with full cream dairy and chocolate. These practices may be customary or a habit but has to be changed in order to limit the extent of acid reflux.
- Consider a calorie-restricted and low GI (glycemic index) diet. While this type of diet may not directly affect the acid reflux, it is crucial for weight loss which is important in the management of GERD.
Foods To Avoid for Acid Reflux
Certain foods are known to decrease the tonicity of the lower esophageal sphincter (LES). The integrity and proper functioning of the LES is crucial to prevent stomach acid from flowing backwards up into the esophagus. Other foods have been implicated in increasing the gastric acid which may contribute to acid reflux.

The foods and drinks that should be avoided include :
- Caffeinated beverages – coffee, tea, colas and certain energy drinks.
- Alcoholic drinks and foods cooked with alcohol.
- Acidic drinks like citrus (orange, lemon and grapefruit), cranberry and some people may be sensitive to tomato juice as well.
- Fatty foods – oily foods, fatty meats, foods with double cream.
- Vegetables like onions, garlic, horse radish, bell peppers (capsicum) and peppadews.
- Spicy foods should be eaten in moderation or avoided altogether.
- Chocolates are widely reported as an irritant and so are mints, although many people find relief with mint sweets after meals.
- Carbonated drinks and ‘gassy foods’ may result in excessive belching which can contribute to acid reflux.
References
- Gastroesophageal Reflux Disease. Medscape
- Acid Reflux in Adults. NIH.gov





